Optimising Outcomes of Very Low Birth Weight Babies
Case study
Background
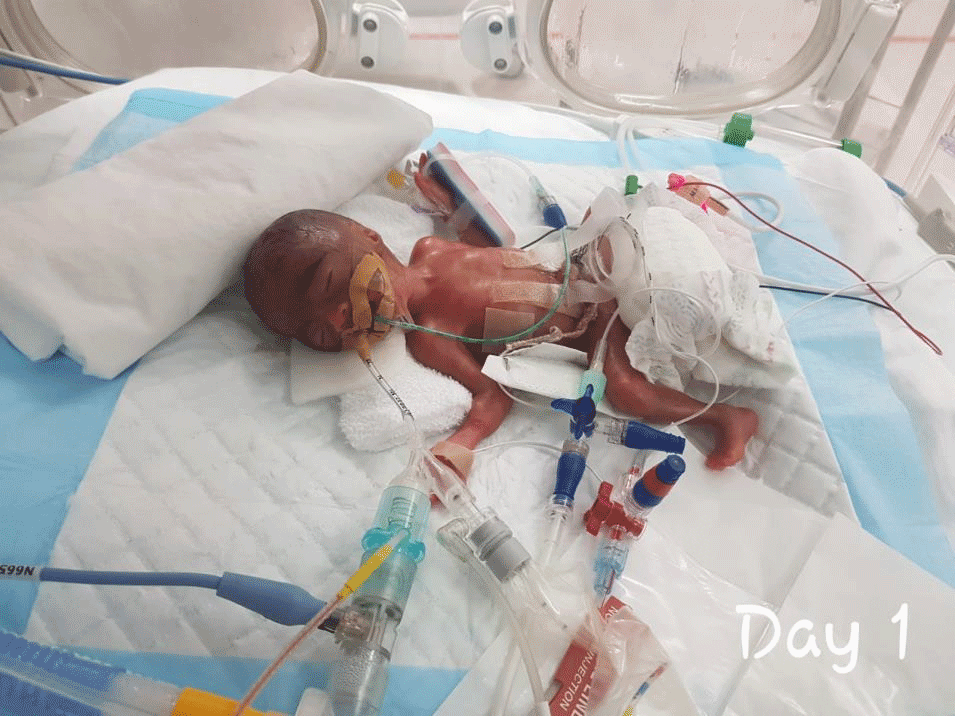
A "Very Low Birth Weight" (VLBW) baby is a premature newborn with a birth weight below 1,500 grams. Cost of care for VLBW babies is very high due to their prolonged stay in Neonatal Intensive Care Units (NICU), high resource utilisation, and potential morbidities such as sepsis, intraventricular hemorrhage, retinopathy of prematurity, chronic lung disease, and necrotising enterocolitis. Every year, 45 to 65 VLBW babies are admitted to the NICU.
Objectives
Improve the quality of care of VLBW babies, as defined by clinical quality index (CQI), and to reduce cost of care.
Methodology
We chose the Value Driven Outcome (VDO) methodology as its underlying philosophy – optimising care while rationalising cost – matches our desired objectives. Value is defined as the level of Quality against a given Cost and expressed as Value = Quality/Cost. VDO allows near-instantaneous monitoring of quality, resource utilisation, and cost; thereby, facilitating implementation of targeted interventions.
We tracked 13 indicators that include a) internationally benchmarked VLBW outcomes, b) resource utilisation, and c) patient experience score. We provide data for four years of intervention (2017–2020) compared against preintervention, baseline years (2015-2016). Baseline data indicated suboptimal patient outcomes in at least three categories: late onset sepsis, chronic lung disease and prolonged hospitalisation due to sub-optimum weight gain. Thus, comprehensive interventions targeted following key areas:
- infection control,
- improving growth through better nutrition,
- prevention of chronic lung disease, and
- staff engagement and education. Families were empowered with education, regular engagement, and active participation during NICU ward rounds.
Quality Indicators - Patient Outcomes
- Length of stay <= 58 Days
- No In-hospital mortality
- No Late onset sepsis
- No Incidence of chronic lung disease (respiratory support at 36 weeks’ postmenstrual age)
- No Incidence of Retinopathy of Prematurity (Stage 3 and above)
- No Incidence of Intraventricular hemorrhage (Grade 3 and above) and periventricular leukomalacia
- No Incidence of Necrotising enterocolitis
- No Readmission rate within 30 days of discharge
Quality Indicators - Resource Utilisation
- Number of x-rays done <= 13
- Number of blood gas done <= 30
- Number of blood glucose done <= 67
- Duration of central lines <= 17 days
Quality Indicators - Patient Experience
- Patient Experience Score >= 8
Results
Clinical Quality Index (CQI)
CQI is the number of patients who met all 13 indicators divided by total number of patients. CQI improved significantly from 13% to 39% between year 2015 to 2019, then dropped slightly to 31% in 2020.
Cost of Care
The cost of patient care reduced significantly in 2018. However, due to combination of factors including a cost-rebase exercise in 2019, cost has increased compared to baseline years.
Quality Indicators
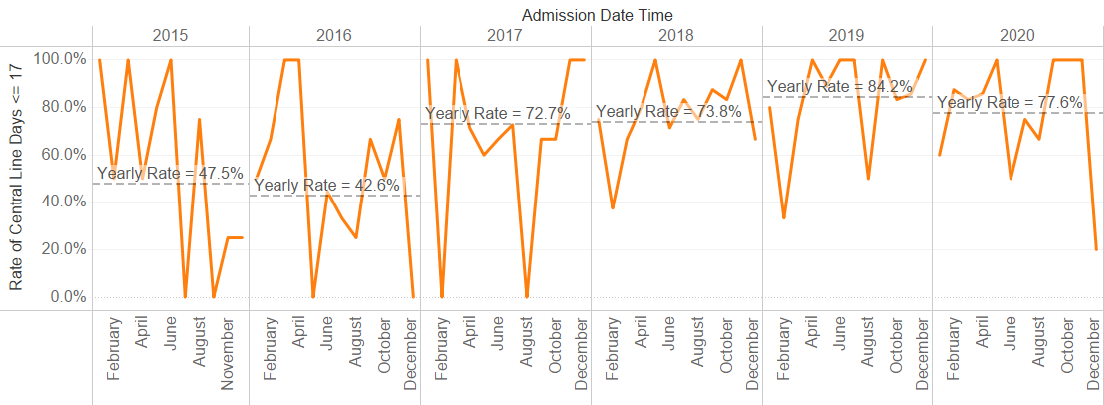
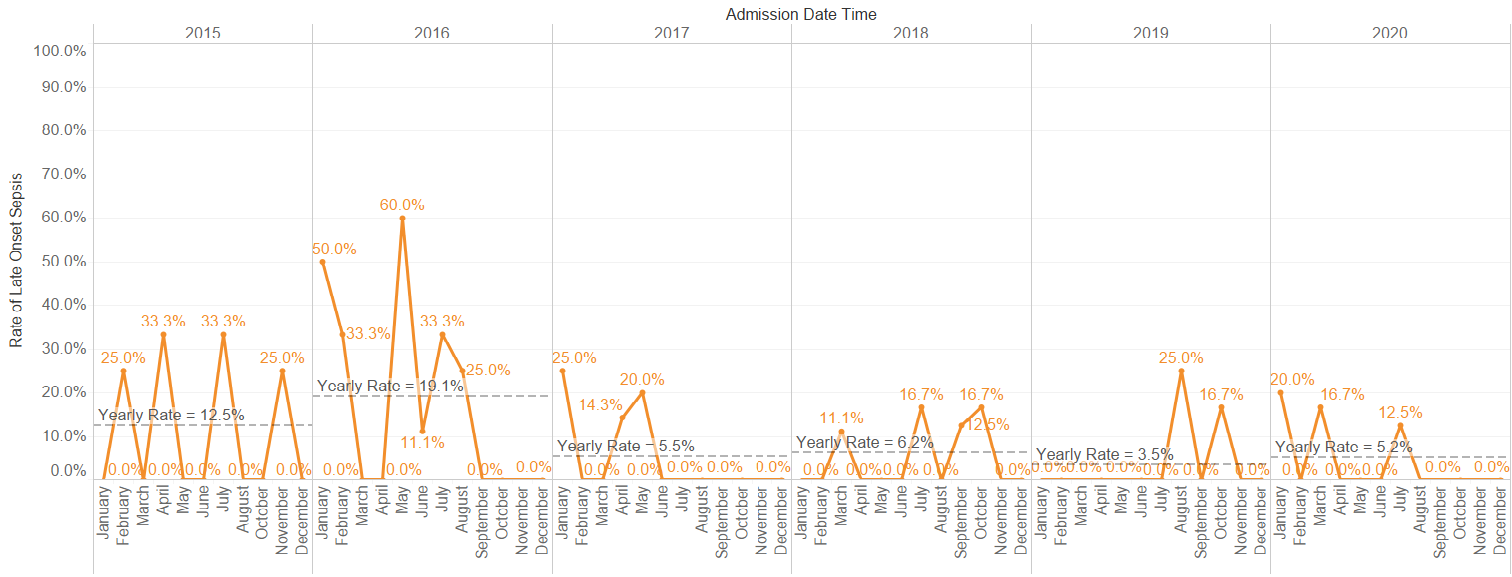
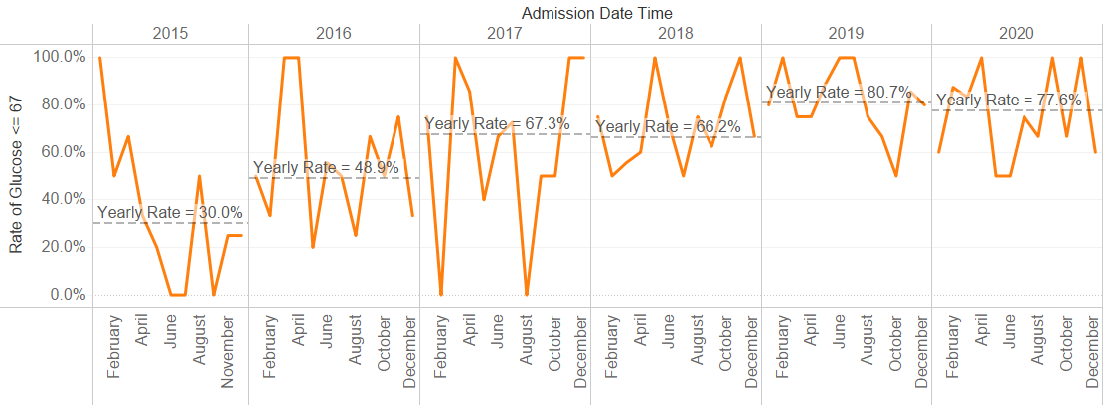
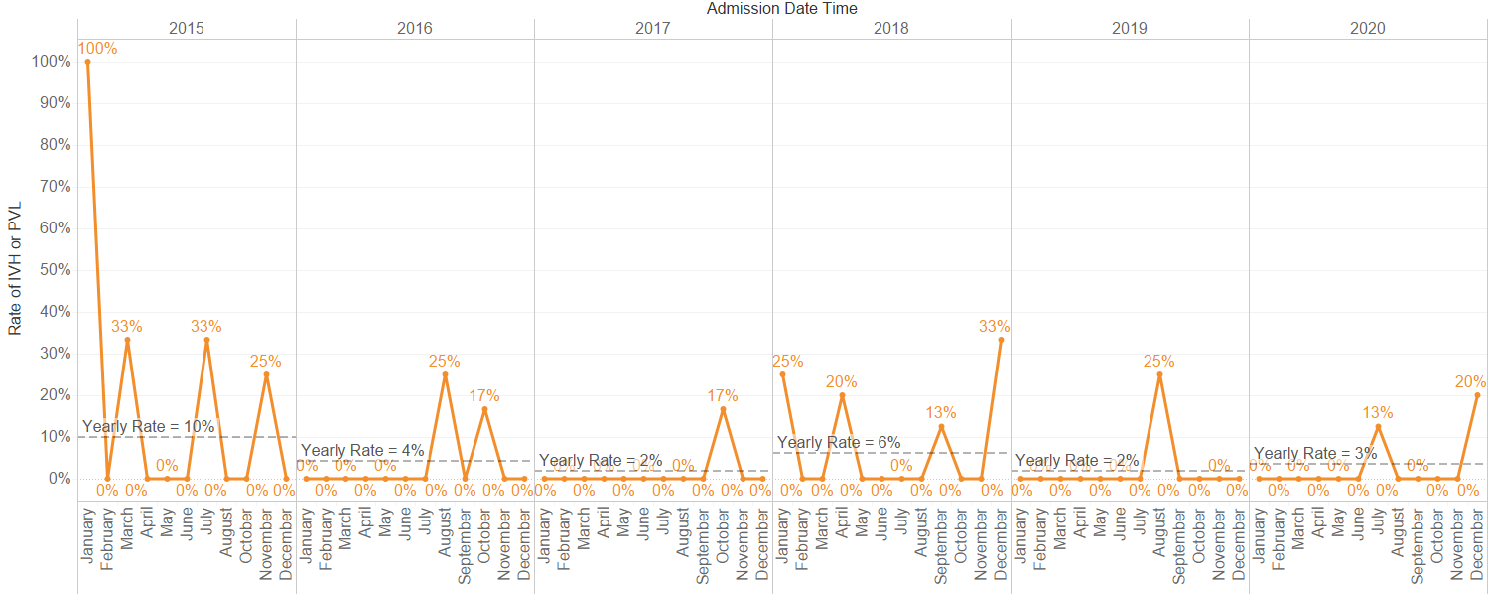
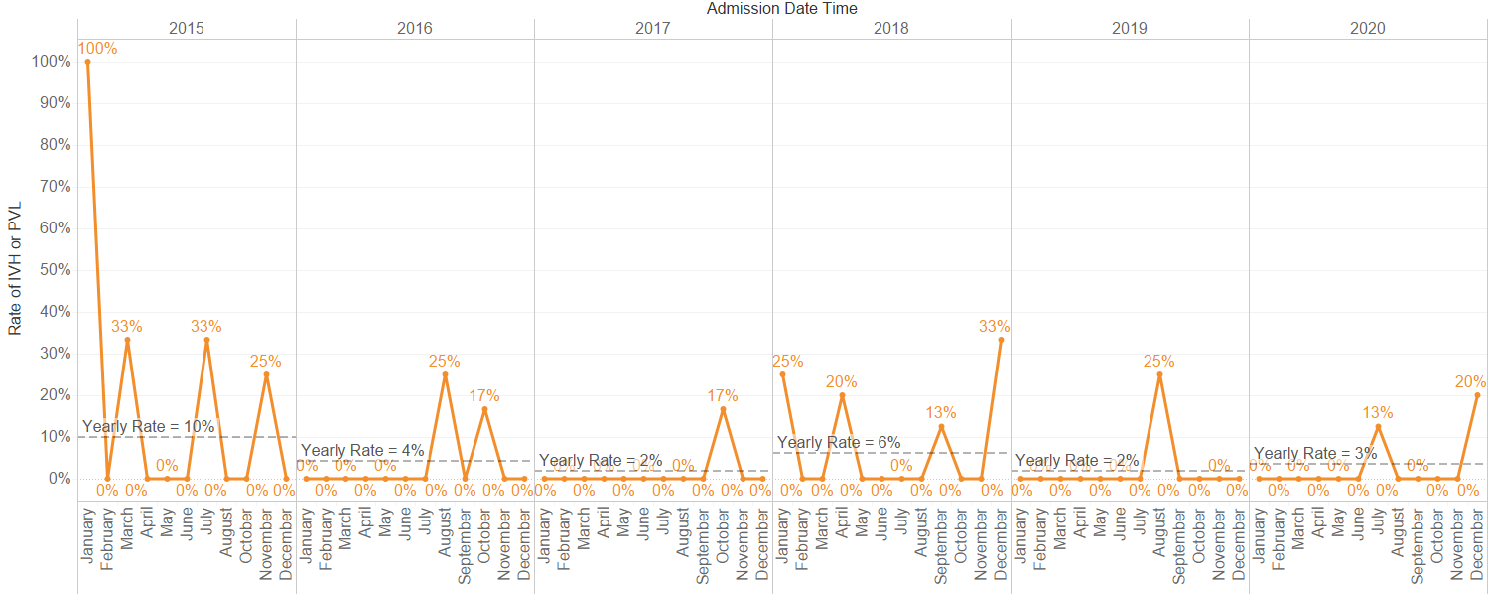
Indicators improved consistently in 4 of 13 categories, from 2015 to 2020: rate of central line days <= 17 days (47.5% to 77.6%); late onset sepsis (12.5% to 5.2%); number of blood glucose done <= 67 (30% to 77%); severe intraventricular hemorrhage & periventricular le ukomalacia (10% to 3%). The incidence of chronic lung disease showed deteriorating trend partly due to improved survival of extreme premature babies. Incidence of retinopathy of prematurity worsened in 2019-2020 to 16.1% and 16.7%. Following that, we instituted several interventions; ongoing monitoring shows severe ROP rate has reduced to 4.7% in 2021.
Fig 1: Rate of central line days <=17 days (2015-2020)
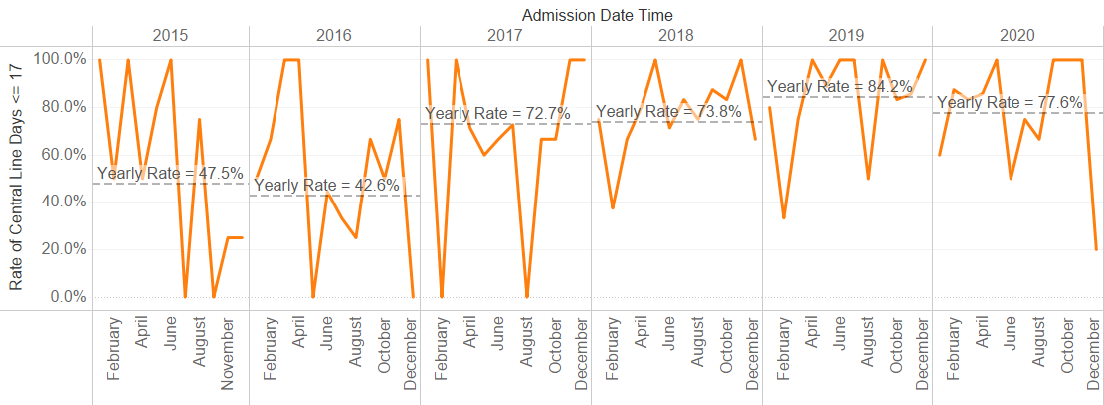
Fig 2: Rate of late onset sepsis (2015 – 2020)
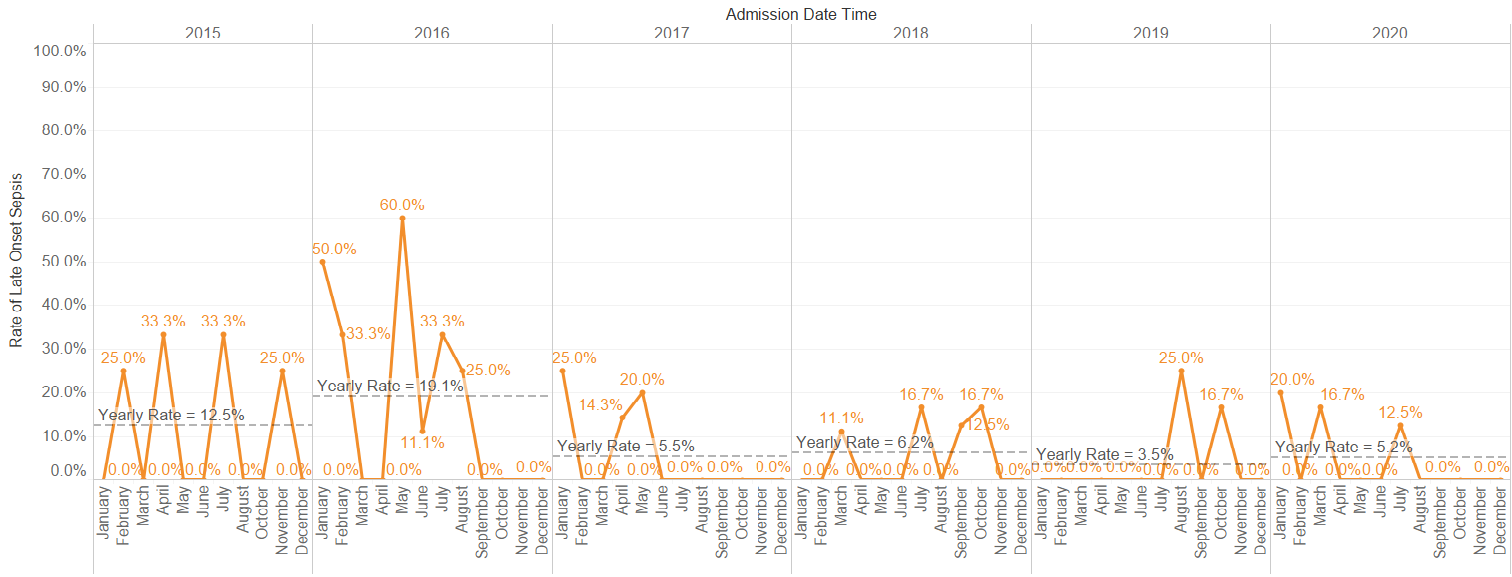
Fig 3: Number of blood glucose done <=67 ( 2015- 2020)
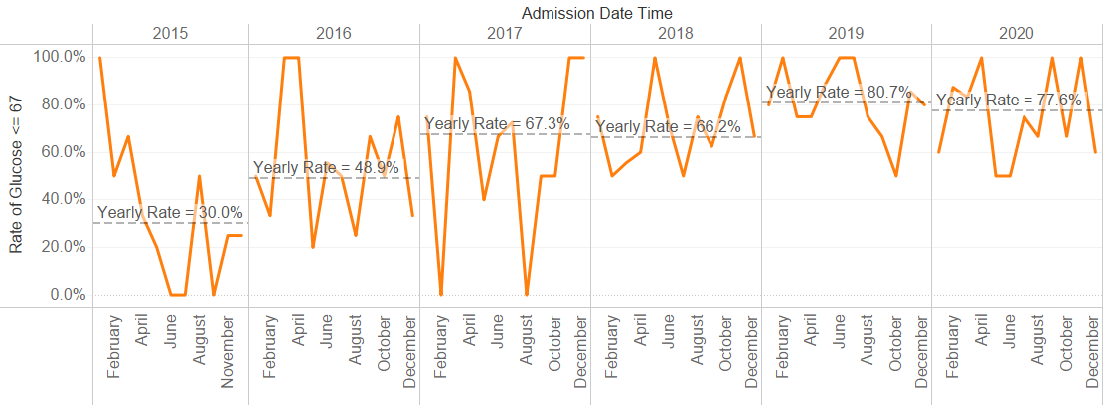
Fig 4: Rate of severe intraventricular hemorrhage and periventricular leukomalacia (2015-2020)
Conclusion
We recognised at the outset that, unlike other VDO projects, the CQI of 100% is unachievable. VLBW babies who are extremely premature (less than 1000g birth weight) are likely to have many morbidities with duration of hospital stay exceeding 58 days. Nevertheless, we demonstrated sustained improvement in CQI and many individual quality indicators from baseline to interventional years through multidisciplinary team effort and parental involvement.