Safety, Feasibility and Healthcare Cost Differences between Inpatient and Outpatient Mobilisation Chemotherapy for Autologous Haematopoietic Stem Cell Transplantation in Multiple Myeloma: A Single Centre Experience
Case study
Background
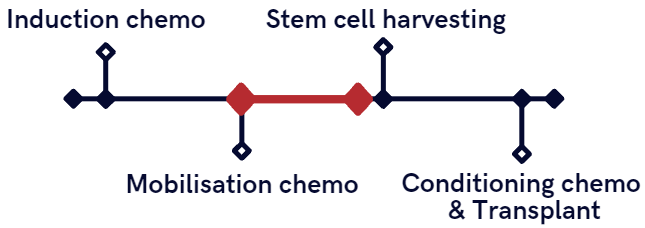
Pre-autologous haematopoietic stem cell transplantation (ASCT) mobilisation chemotherapy for multiple myeloma (MM), vinorelbine and high dose cyclophosphamide (VC), has been historically given inpatient (IP). Our team has offered eligible patients the option of outpatient (OP) VC since 2018 to address rising bed occupancy rates and patients' preferences.
Objectives
Our study aims to audit the feasibility and safety of this initiative, and review potential healthcare related cost savings.
Methodology
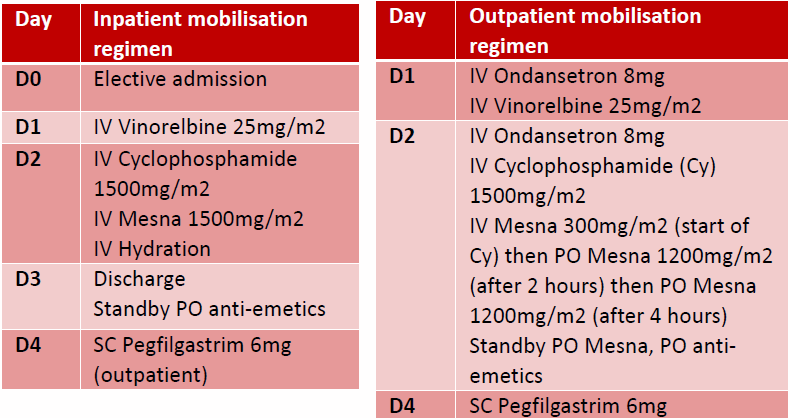
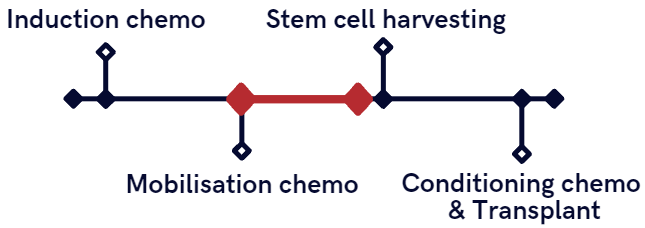
Eligibility criteria and modifications for an OP chemotherapy regimen were developed by a multidisciplinary team (Figure 1).
Figure 1
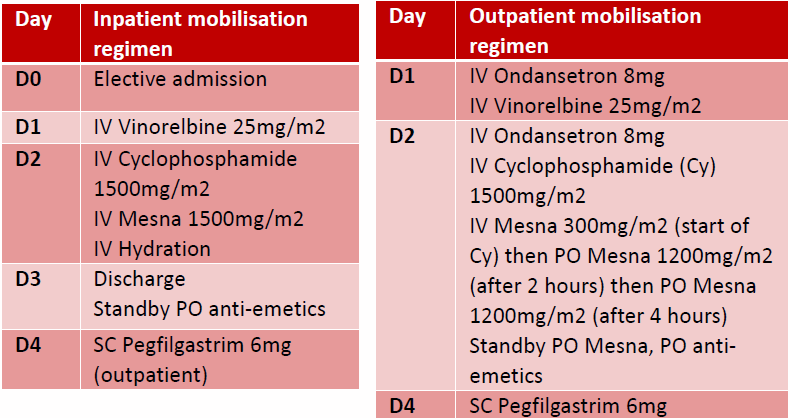
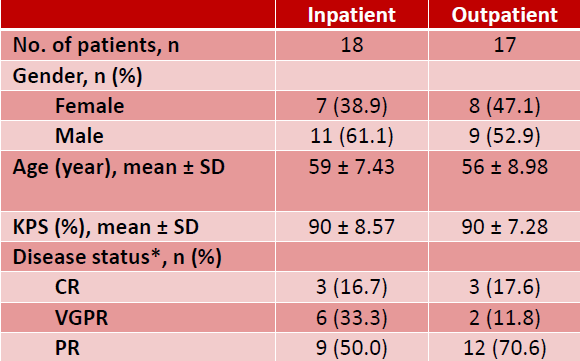
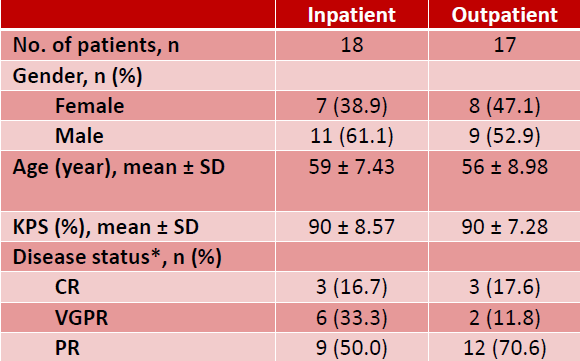
35 MM patients who received VC from 2018 to 2019 were included in our analysis (Table 1).
Table 1. Patient characteristics
Outcome measures including unexpected complications and unplanned admissions were compared between IP and OP.
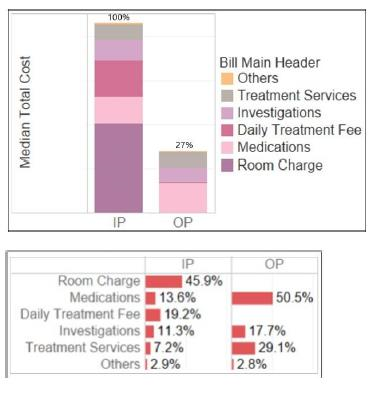
Using Value Driven Outcome (VDO) analysis, costs incurred were calculated from the start of VC to the day before admission for harvest (Figure 2).
Figure 2
Results
Safety
There was no increase in unexpected clinical complications or unplanned admissions in the OP cohort compared to the IP cohort. 3 IP presented to the emergency room (ER) with symptoms attributed to granulocyte colony stimulating factor (G-CSF). 2 were admitted and proceeded with planned stem cell harvesting the next day, while 1 was discharged and readmitted the next day for harvesting. 2 OP presented to the ER. 1 had symptoms attributed to G-CSF and 1 had upper respiratory tract infection symptoms. Both were admitted and proceeded with planned stem cell harvesting the next day.
Benefits
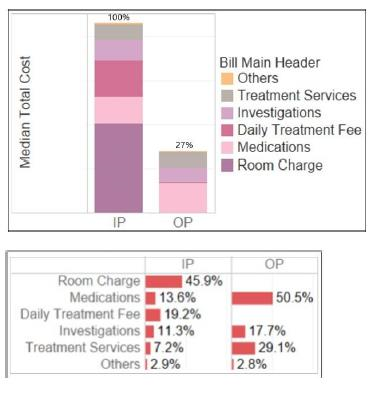
There was an approximate savings of 51 hospital bed days over 2 years from OP VC. The median cost (Figure 3) was 73% lower in the OP cohort. The difference was mainly due to certain costs not incurred in the OP setting.
These included:
- Room charges and daily treatment fees (which accounted for an average of 46% and 19% of IP charges respectively).
- Inpatient investigations such as methicillin-resistant Staphylococcusaureus (MRSA) screening.
There was no significant difference in the cost of medications used for the OP and IP regimens.
Figure 3. Cost comparison between IP and OP mobilisation chemotherapy
Conclusion
Our findings show that OP mobilisation chemotherapy for MM is safe, feasible and associated with improved bed utilisation and cost savings. This supports the ongoing paradigm shift of right-siting treatment services from the IP to OP setting, so as to optimise utilisation of healthcare resources.