Peritoneal Metastasis is difficult to treat and is best managed by a multi-disciplinary team that includes surgeons and medical oncologists.
Systemic Chemotherapy
Chemotherapy drugs given intravenously or sometimes in combination with oral tablets circulate through the whole body. This type of treatment is suitable for cancers that have metastasised to multiple parts of the body.
Cytoreductive Surgery (CRS) with Hyperthermic lntraperitoneal Chemotherapy (HIPEC)
CRS is an extensive surgery that removes all visible cancers within the abdominal cavity. At the end of CRS, a heated chemotherapy solution is applied in the peritoneal cavity to destroy the remaining cancer cells that cannot be seen with the naked eye.
Intra-peritoneal (IP) Chemotherapy
IP chemotherapy (Figure 3) is injected into the peritoneal cavity via an intraperitoneal port that is inserted via keyhole surgery. The port is buried under the skin and connected to a catheter that enters the peritoneal space.
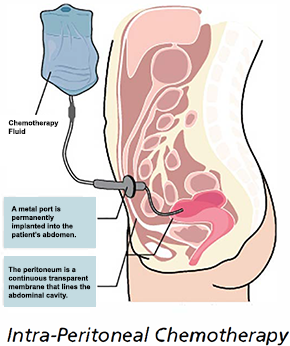
Figure 3: Set-up of IP Chemotherapy
Pressurised Intra-Peritoneal Aerosol Chemotherapy (PIPAC)
PIPAC (Figure 4) is a novel method of delivering chemotherapy directly into the peritoneal cavity in an aerosol form. It utilises the physical properties of pressurized gas to distribute the drug evenly and deeply. This allows greater penetration of the drug into the cancer cells, with reduced systemic side effects of the chemotherapy agent. PIPAC is performed as a short and simple laparoscopic (keyhole) surgery. Under general anaesthesia, small instruments will be placed into the abdomen. A micro-pump will deliver the chemotherapy drug into the peritoneal cavity as an aerosol. At the end of the procedure, any residual gas within the peritoneal cavity will be removed.
Currently, PIPAC is a minimally-invasive palliative procedure that aims to prolong survival and preserve quality of life. Due to the low dosage applied, PIPAC can be combined with systemic palliative chemotherapy and has minimal organ toxicity. This procedure can be repeated at intervals of six weeks to three months.
 Figure 4: Set-up of Pressurised Intra-Peritoneal Aerosol Chemotherapy (PIPAC)
Figure 4: Set-up of Pressurised Intra-Peritoneal Aerosol Chemotherapy (PIPAC)

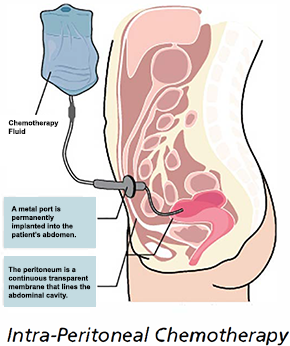
 Figure 4: Set-up of Pressurised Intra-Peritoneal Aerosol Chemotherapy (PIPAC)
Figure 4: Set-up of Pressurised Intra-Peritoneal Aerosol Chemotherapy (PIPAC)













