There are now several curative treatment modalities for HCC in selected patients. These include radiofrequency ablation (RFA), surgery and liver transplantation. There are also a host of other treatment modalities used in more advanced stages of HCC including transarterial chemoembolisation (TACE), Yttrium-90 radioembolisation (Y-90), stereotactic body radiation therapy and molecular targeted therapies such as sorafenib, regorafenib and levantinib as well as immunotherapy. In addition, there are numerous clinical trials available for patients with advanced stage HCC.
Surgical Resection
Surgery is suitable for patients with early stage HCC and well preserved liver function who would tolerate a proportion of their liver being removed.
Liver Transplantation
Patients transplanted for early to intermediate stage HCC have five year survival rates exceeding 73%. Liver transplantation not only provides a cure for HCC but also for the underlying liver disease.
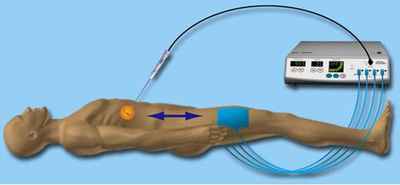
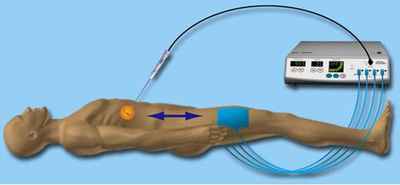
Radiofrequency Ablation (RFA)
RFA is suitable for patients with small to intermediate size HCCs. A small electrode needle is inserted into the tumour through a small puncture in the skin. An electric current passed through the electrode allows complete ablation of the tumour.
Transarterial Chemoembolisation (TACE)
TACE is a minimally invasive procedure performed by experienced radiologists under X-ray imaging. An injection at the groin or wrist is administered to allow the insertion of a small caliber tube into the blood vessel(s), supplying the liver cancer cells, to deliver chemotherapeutic medication to the cells. Thereafter, this blood vessel(s) supplying the liver cancer will be blocked to deprive the cancer cells of blood supply and induce their death.

Yttrium-90 Radioembolisation (Y-90)
Y-90 is a technique whereby radioactive beads are deployed into the tumour via a blood vessel. The radioactive beads emit low-energy radioactivity that kills the tumour.
Molecular targeted therapy
Many targeted therapeutic agents such sorafenib, regorafenib and levantinib are available for patients with advanced stage HCC to prolong their lives.
Immunotherapy
This group of medications will assist our body immune system to target and control HCC tumour cells.
Patients treated for HCC are followed-up on a regular basis for surveillance of any tumour recurrence.