In the acute/emergency setting:
- Optimise lung function, e.g. supplemental oxygen
- Medications to help remove excess fluid in body (Diuretics)
- Pain relief
- Medications to correct arrhythmias
- Medications to stimulate the heart to pump
In the long term:
- Starting on drugs that have been shown to reduce mortality and morbidity in heart failure patients (e.g. Angiotensin converting enzyme inhibitors, beta blockers, spironolactone)
- Drugs for symptom relief (e.g. diuretics)
- Control of risk factors (e.g. optimise diabetic control, hypertension)
- Regular monitoring of clinical status of heart failure patients
Procedures that can help heart failure patients include:
- Percutaneous Transluminal Coronary Angioplasty (PTCA)
- Coronary bypass grafting
- Valve surgery
- Heart transplantation
Treatment modalities are very much dependent on the patient: how is his condition currently, what he was like before, and what precipitated the heart failure. The doctor will be able to advise on the best method to manage heart failure in the long run based on the whole picture.
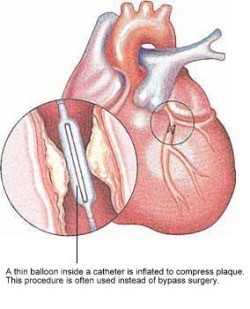
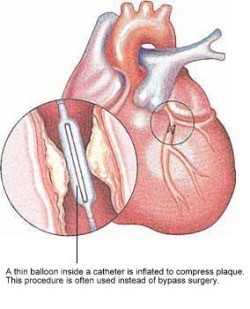
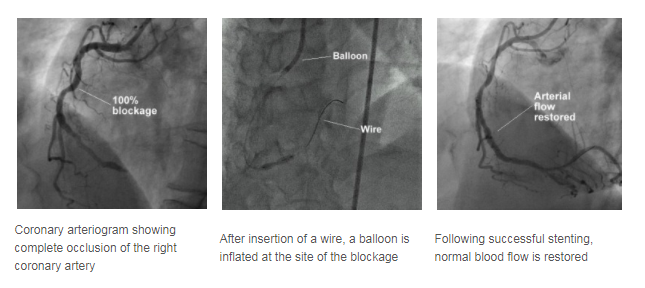
Coronary Angioplasty and Stenting
Coronary artery narrowings may be treated using either medications that reduce the heart's demand for blood, or by procedures aimed at increasing the heart's blood supply. One of the two most common methods to increase the blood supply is coronary angioplasty, sometimes abbreviated as PTCA (Percutaneous Translunimal Coronary Angioplasty).
PTCA offers a non-surgical alternative to Coronary Artery Bypass Surgery.
In PTCA, a balloon mounted on a thin tube (a catheter) is advanced into your coronary artery until it lies within the narrow area. The balloon is then inflated at high pressure, often a few times, to dilate the narrowing. Upon balloon deflation, the arterial narrowing is often significantly reduced.
A stent is a small metal coil to provide support to the narrowed segment of the coronary artery after angioplasty, preventing the artery from collapsing and reducing the likelihood the narrowing will recur. Modern stents are made of stainless steel or a cobalt chromium alloy and are inert to the body. Some stents also have a medication coating and these may be preferred in certain situations to further reduce the chance of repeat narrowing of the heart arteries. Nowadays, stents are frequently placed directly over the narrowed segments (direct stenting) without prior balloon dilatation.

A stent is a small metal coil that provides support to the
narrowed segment of the coronary artery after angioplasty
What to expect?
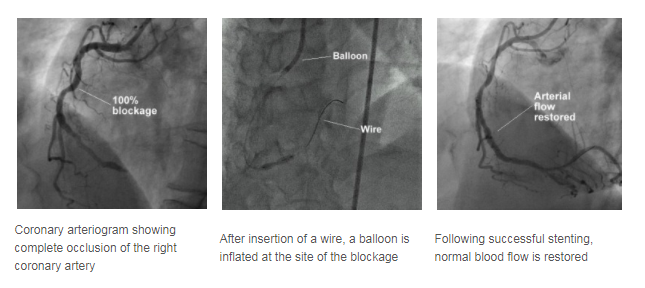
Before going through a PTCA, a coronary angiogram is done first to provide a 'roadmap'. Undergoing PTCA is also very similar to having a coronary angiogram procedure.
- First, you will be injected with local anaesthetic.
- A plastic tube known as sheath is inserted in a large artery in the groin or wrist. Through this sheath, a catheter is advanced to the mouth of the narrowed coronary artery.
- A thin wire is then threaded through the catheter and positioned in the coronary artery.
- Over this wire, the balloon catheter is pushed into the artery and the balloon positioned over the area of narrowing.
During balloon inflation, you may experience some chest discomfort, and you should report this to your attending cardiologist. Stenting is carried out in a similar manner. The procedure may take 1 to 2 hours or more depending on the complexity of the diseased artery.
Following the successful PTCA, you will be monitored in a special monitoring ward. During this period, the sheath may be kept in your groin artery for 4 to 5 hours. However, the sheath may be removed immediately after the procedure if the situation allows. After the sheath is removed, the puncture site will be compressed for about 30 minutes to ensure that there is no bleeding.
You will have to remain in bed for several hours or until the following day to ensure the puncture site is sufficiently healed before walking. Your cardiologist will determine how long you need to stay in bed before you can walk around. Following that, some blood tests and ECGs will be performed to monitor your condition. If there are no complications, most patients can be discharged on the same day or the day after.
What to prepare?
- Please inform your doctor of any allergy, in particular, allergies to seafood, iodine, X-ray contrast medium and pain relieving medications.
- Please inform your doctor if you have a history of peptic ulcer disease, recent strokes, or bleeding tendencies.
- If you are suffering from diabetes mellitus and you are taking a medication called metformin, please inform your doctor and you would need to stop this particular medication for at least 2 days before and after angiography.
- Upon discharge, you will be given two anti-blood clotting medications - aspirin and either ticlopidine or clopidogrel. Your cardiologist will advise you on the optimal length of time you should continue taking the latter two medicines (ticlopidine or clopidogrel), which can range from one month to one year. However, aspirin should be taken indefinitely to prevent future heart attacks, unless instructed by your cardiologist.
What are the success rates?
The success rate of coronary angioplasty is usually about 95%, depending on the nature of your coronary narrowing. However, in about 5% of cases, the procedure may be unsuccessful and the artery remains narrowed. In very few patients (about 1%), urgent bypass surgery may be required if the procedure is complicated.
There is a possibility of a recurrence of the narrowing of the coronary artery in the 6 months following the initial successful angioplasty or stenting, and you would usually feel a chest discomfort should it happen. If you feel a chest pain, you should seek medical attention immediately and inform your doctor.
What are the potential risks or complications?
Major complications like heart attacks, abnormal heart rhythm, stroke and death occur in less than 1% of the patients undergoing PTCA.
Less serious complications like bleeding from the puncture site, bruising and swelling of the puncture site, and blood clot formation in the artery where the sheath is insert occur in 1-3% of the patients.
Overall, the procedure is very safe and well-tolerated.
Home Care
As a patient:
- Resume normal daily activities.
- Notify the doctor at once if you experience bleeding or increase bruising at the puncture site; or when you experience a recurrence of symptoms, such as breathlessness or decreased exercise tolerance.
- Comply with regular follow-up visits.
Coronary Artery Bypass Surgery Grafting (CABG)
What is it?
Unlike a traditional Coronary Artery Bypass Surgery, the off-pump CABG does not require the use of the heart-lung machine. Instead of stopping the heart, surgeons can now hold portions of the heart stable during surgery due to technological advances and new kinds of operating equipment. The surgeon can now bypass the blocked artery in a highly controlled and stabilised environment while the rest of the heart continues pumping blood to the rest of the body.
Why do you need this surgery?
Only certain patients with Coronary Artery Disease can receive this surgery. At present, this procedure can be performed on all the arteries of the heart.
It would ideal for you if you are at an increased risk for complications from the traditional bypass. Coronary Artery Bypass Surgery will be an option if you have the conditions below:
- Heavy Aortic Calcification
- Carotid Artery Stenosis
- Prior Stroke
- Compromised Pulmonary or renal function
How should you prepare for the surgery?
- Stop smoking. You should stopbecause smoking is a risk factor for coronary heart disease. Your heart disease will not improve if you continue to smoke. It also increases your risk of complications from the surgery.
- Talk to your doctor or other people who have had the surgery. Knowing what to expect may help reduce your anxiety before the operation.
- Plan for your care and recovery after the operation. Allow for time to rest, and try to get help for your day-to-day activities.
What happens during the surgery?
- You will be asked to put on a surgical gown on the morning of your operation.
- General anaesthesia will be given to you and you will be asleep for the entire operation.
- Your breast bone will be divided.
- If more than one artery has to be bypassed, a vein from your leg will be removed and prepared for the additional bypass.
- A stabilising device is placed on the surface of your heart to limit the motion of the beating heart.
- The coronary arteries are opened beyond the sites of the blockage, and the open ends of the vein graft are sewn to the openings.
- Blood flow is then established.
- The heart is effectively "bypassed".
- Drainage catheters placed around the heart are usually removed after 24 hours.
What are the potential risks or complications?
- There are always some risks when you have general anaesthesia. Discuss these risks with your doctor.
- There is a risk of infection or bleeding from this operation.
- New blockages can develop in the bypassed vessels. This might require another heart catheterisation and surgery. It is important to make changes to your lifestyle to decrease the risk of blockage.
- There is a risk of getting a stroke during and after the operation.
What happens after the surgery?
- Temporary pacing wires will be placed to regulate your heart rate and will be removed just before you are discharge.
- You will be recovering in the CCU (Coronary Care Unit) after the surgery where you will receive specialised care and monitoring.
- Usually, you will be transferred to the normal ward the next day.
Home Care
- Have a relative or friend to pick you up on the day of your discharge.
- You will not need nursing at home, but it will be good to have someone help you with your shopping and also to support you for the first 10 days or so.
- Follow up with the pre-arranged check up at the hospital with your doctor.
- Full recovery should take about 3 months.