If you are outside of a hospital:
- Immediately call for an ambulance
- Take an aspirin tablet if available
Once in a hospital:
- All the relevant tests will be carried out once you are stabilised. Pain relief will be provided.
- ECG: a specific pattern will arise from the tracings of the electrical activity of the heart.
- Blood tests: the level of cardiac enzymes will rise above normal in the event of a myocardial infarct, due to injury/death of the heart muscle cells. The degree of abnormality on the ECG and the cardiac enzymes can be used to roughly gauge the amount of heart muscle that was damaged during the infarct.
The heart muscles that were affected during a myocardial infarct do not die off immediately. If the flow of blood and hence oxygen is restored to these muscles as soon as possible (within a few hours), much of the muscle cells will survive. This is the reason for prompt treatment. There are two ways in which this can be achieved:
- Thrombolysis: This method uses medications that can break down any clots that are the cause of the myocardial infarct, and in doing so, allow reperfusion of the infarcted heart muscles. These agents can achieve reperfusion in 50-70% of patients if administered as soon as possible, to reduce mortality and morbidity. Thrombolysis carries with it risks, including increased risks of haemorrhage (bleeding). Therefore, it will be unsuitable in patients who have had a recent major bleed, stroke, uncontrolled hypertension, recent surgery or bleeding disorders.
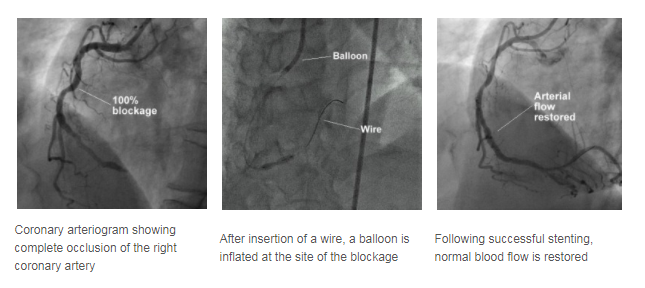
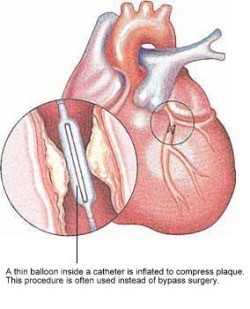
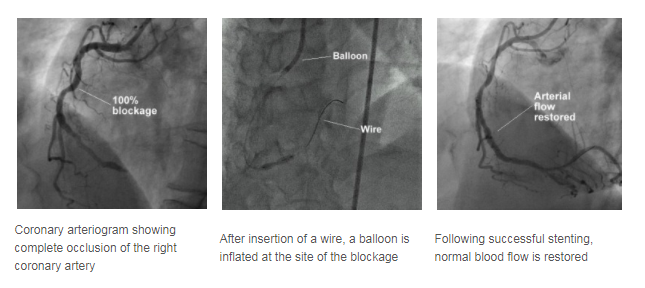
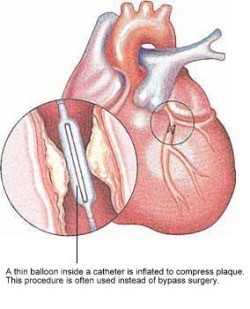
- Angioplasty: A thin wire with a balloon at the end will be passed into the blocked coronary artery via a vessel in the groin or arm. The balloon is then inflated inside the blocked/narrowed artery to widen it, allowing blood to flow again. A stent may be placed as well to keep the vessel widened.
As there may be increased risks of fatal heart arrhythmias developing after a Heart Attack, you may be transferred to the Coronary Care Unit (CCU) for closer monitoring and intervention if required. ECGs and blood tests will be carried out over the course of your stay to monitor your progress.
Once you are fit for discharge, you will need to control the risk factors of heart disease, such as stopping smoking, optimising diabetic control, and controlling the cholesterol levels in the blood. Drugs are also commonly prescribed to prevent a further myocardial infarct, and examples of them are aspirin (to make the blood "thinner" to prevent blood clots from forming), and a beta blocker (slows the heart rate down).
Coronary Angioplasty and Stenting
Coronary artery narrowings may be treated using either medications that reduce the heart's demand for blood, or by procedures aimed at increasing the heart's blood supply. One of the two most common methods to increase the blood supply is Coronary Angioplasty, sometimes abbreviated as PTCA (Percutaneous Translunimal Coronary Angioplasty).
PTCA offers a non-surgical alternative to Coronary Artery Bypass Surgery.
In PTCA, a balloon mounted on a thin tube (a catheter) is advanced into your coronary artery until it lies within the narrow area. The balloon is then inflated at high pressure, often a few times, to dilate the narrowing. Upon balloon deflation, the arterial narrowing is often significantly reduced.
A stent is a small metal coil to provide support to the narrowed segment of the coronary artery after angioplasty, preventing the artery from collapsing and reducing the likelihood that the narrowing will recur. Modern stents are made of stainless steel or a cobalt chromium alloy and are inert to the body. Some stents also have a medication coating and these may be preferred in certain situations to further reduce the chance of repeat narrowing of the heart arteries. Nowadays, stents are frequently placed directly over the narrowed segments (direct stenting) without prior balloon dilatation.

A stent is a small metal coil that provides support to the
narrowed segment of the coronary artery after angioplasty.
What to expect?
Before going through a PTCA, a coronary angiogram is done first to provide a 'roadmap'. Undergoing PTCA is also very similar to having a coronary angiogram procedure.
- First, you will be injected with local anaesthetic.
- A plastic tube known as sheath is inserted in a large artery in the groin or wrist. Through this sheath, a catheter is advanced to the mouth of the narrowed coronary artery.
- A thin wire is then threaded through the catheter and positioned in the coronary artery.
- Over this wire, the balloon catheter is pushed into the artery and the balloon positioned over the area of narrowing.
During balloon inflation, you may experience some chest discomfort, and you should report this to your attending cardiologist. Stenting is carried out in a similar manner. The procedure may take 1 to 2 hours or more depending on the complexity of the diseased artery.
Following the successful PTCA, you will be monitored in a special monitoring ward. During this period, the sheath may be kept in your groin artery for 4 to 5 hours. However, the sheath may be removed immediately after the procedure if the situation allows. After the sheath is removed, the puncture site will be compressed for about 30 minutes to ensure that there is no bleeding.
You will have to remain in bed for several hours or until the following day to ensure the puncture site is sufficiently healed before walking. Your cardiologist will determine how long you need to stay in bed before you can walk around. Following that, some blood tests and ECGs will be performed to monitor your condition. If there are no complications, most patients can be discharged on the same day or the day after.
What to prepare?
- Please inform your doctor of any allergy, in particular, allergies to seafood, iodine, X-ray contrast medium and pain relieving medications.
- Please inform your doctor if you have a history of peptic ulcer disease, recent strokes, or bleeding tendencies.
- If you are suffering from diabetes mellitus and you are taking a medication called metformin, please inform your doctor. You will need to stop taking this particular medication at least 2 days before and after angiography.
- Upon discharge, you will be given two anti-blood clotting medications - aspirin and either ticlopidine or clopidogrel. Your cardiologist will advise you on the optimal length of time you should continue taking the latter two medicines (ticlopidine or clopidogrel), which can range from one month to one year. However, aspirin should be taken indefinitely to prevent future heart attacks, unless instructed by your cardiologist.
What are the success rates?
The success rate of coronary angioplasty is usually about 95%, depending on the nature of your coronary narrowing. However, in about 5% of cases, the procedure may be unsuccessful and the artery remains narrowed. In very few patients (about 1%), urgent bypass surgery may be required if the procedure is complicated.
There is a possibility of a recurrence of the narrowing of the coronary artery in the six months following the initial successful angioplasty or stenting, and you would usually feel a chest discomfort should it happen. If you feel a chest pain, you should seek medical attention immediately and inform your doctor.