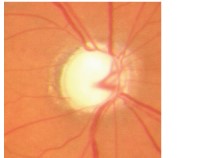
Glaucoma is an eye condition where damage to the optic nerve results in the gradual loss of vision. The optic nerve in each eye serves to transmit images from our retina to our brain. Usually, but not always, damage to the optic nerve in is caused by high pressure within the eyeball.
Sometimes called the "silent thief of vision", Glaucoma often causes irreversible harm to the eyes before there is any vision loss. Without treatment, glaucoma can lead to blindness.
In Singapore, Glaucoma affects about 3 per cent of those aged over 40. This risk increases with age.
How does Glaucoma occur?
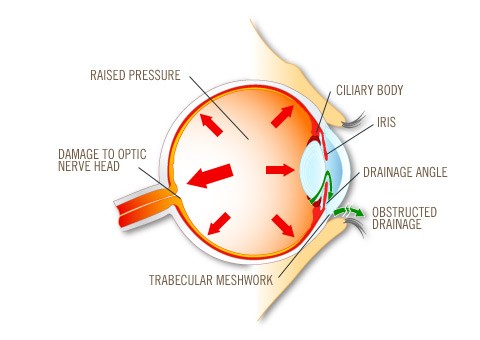
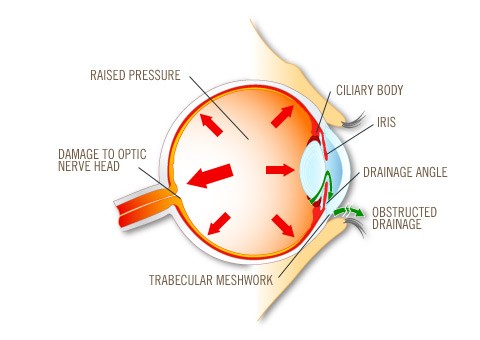
The eye is like a ball filled with fluid which provides oxygen and nourishment to the rest of the eye. It has an inflow tap (ciliary body) and an outflow drain (trabecular meshwork).
To maintain normal pressures, the inflow must balance the outflow. In certain types of Glaucoma, such as Angle Closure Glaucoma, if the drainage is blocked, fluid accumulates and pressure in the eye builds up. This raised pressure may damage the optic nerve.
Glaucoma can be classified into primary (not associated with other eye diseases) and secondary (as a result of pre-existing eye diseases). These are sub-divided into Open-Angles and Closed-Angles Glaucoma.
Primary Open-Angle Glaucoma
This is the most common type of Glaucoma. Its symptoms are usually gradual and you may not notice any vision loss until the advanced stages. Primary Angle-Closure Glaucoma may be be acute or chronic.
Acute Primary Angle-Closure Glaucoma
- Occurs more commonly in the middle-aged or elderly, especially those who are long-sighted.
- Characterised by a sudden increase in the eyeball pressure, causing sudden onset of pain, redness and blurred vision in one or both eyes. There may be headache, nausea and vomiting as well.
- Urgent treatment to lower the pressure is essential to save vision.
Chronic Primary Angle-closure Glaucoma
- Vision loss is progressive with side vision usually being affected first.
- The disease is often very advanced before visual loss is noted, that is why this disease is often called the "silent thief of vision".
In both forms of Glaucoma, laser treatment (peripheral iridotomy), along with anti-Glaucoma eye drops may be needed.
Secondary Glaucoma occurs when other eye diseases cause an increase in eye pressure, leading to optic nerve damage. This can be related to other medical conditions such as diabetes mellitus, or can happen following injury to the eye.
One can also be born with Glaucoma, in the case of Congenital Glaucoma.
Normal Tension Glaucoma
In Normal-Tension Glaucoma, susceptible individuals develop optic nerve damage even when their eye pressures are within normal limits.
Risk factors for the development of Normal-Tension Glaucoma include:
- Family history of Glaucoma
- History of major blood loss or blood transfusion
- History of migraine
- History of Raynaud's phenomenon- spasm of blood vessels leading to discolouration of fingers and toes.
Treatment with anti-Glaucoma eye drops is first line for this condition.