What you will need to perform a finger-prick test?
- A blood glucose meter
- Glucose test-strips
- Finger prick device (lancing device)
Which blood glucose meter should you use?
There are various types of blood glucose meters (glucometers) available in pharmacies. Your healthcare team can help you in selecting the most suitable meter for your needs and guide you on how to use it.
Some features you can look out for when choosing a glucose meter:
- Ease of use
- Small volume of blood needed
- Accuracy of reading
- Speed in obtaining reading
- Cost of glucose test-strips
How to perform a finger-prick sugar test?
- Wash hands with soap and water, and dry thoroughly.
- Insert the test strip into the meter.
- Squeeze your finger, then use the lancing device to prick the side of your finger.
- Squeeze out a drop of blood. Ensure the drop is sufficient.
- Apply a single drop of blood to the edge of the test strip.
- Take note of your blood sugar reading.
When and how often should you monitor?
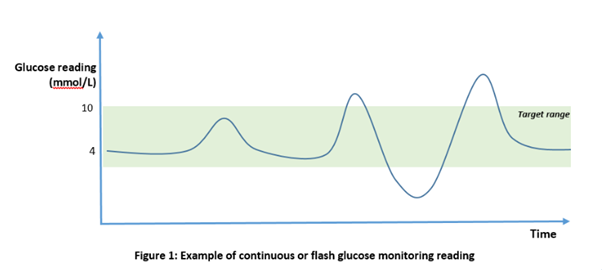
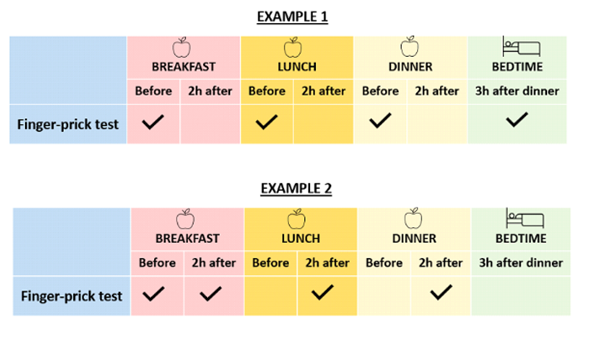
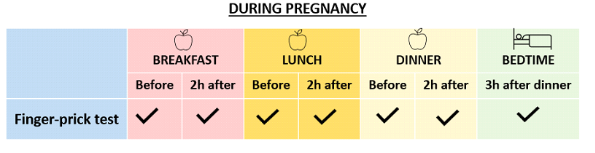
Performing blood sugar testing in a structured manner helps you identify patterns so you can better understand what needs to be changed to achieve better sugar levels.
Structured testing is more useful than random testing. For instance, taking a pre-meal blood sugar reading provides a baseline before eating, while a two-hour post-meal reading reveals how your blood sugar levels respond to the food consumed.
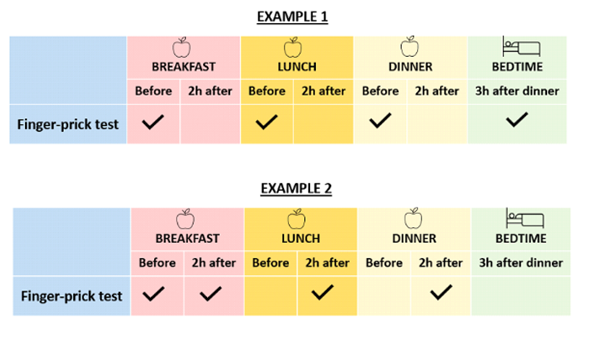
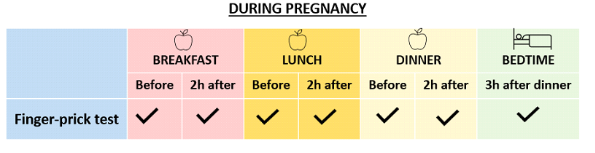
Some examples of timings are shown below. Discuss with your healthcare team the best schedule and frequency for performing finger-prick testing for you.
Additionally, you should check your blood sugar levels:
- When you experience symptoms of low blood sugar
- When you experience symptoms of high blood sugar
- Before, during, and after exercise or other important activities (e.g. driving), especially if you are prone to low blood sugar episodes
- When you are unwell
What is your target blood sugar level?
Everyone is unique, so your blood sugar targets may differ from others. Discuss with your healthcare team to determine your personal blood glucose targets, so you can work towards them safely.
An example of blood glucose targets for finger-prick testing -
| Timing | Target |
|---|
| Before meals | 4 to 7 mmol/L |
| Two hours after a meal | Less than 10 mmol/L |
| Before bedtime | 6 to 8 mmol/L |
Our top tips for a less painful finger-prick test include the following:
- Choose a lancing device that you are most comfortable with. Consult your healthcare team for recommendations.
- Adjust the penetration depth of your lancing device. Set it to the smallest number required to obtain a good drop of blood.
- Avoid pricking the thumb and index finger.
- Use the side of the finger where there are fewer nerve endings, not the tips.
- Test on a different finger or a different part of the finger each time. Rotate testing sites to allow time for healing.
- Change your lancets regularly.