CHD is an abnormality of the structure of the heart that exists at birth. It occurs when the heart or major blood vessels fail to develop or mature normally during the pregnancy.
The list below describes some terms commonly used in CHD:
- Stenosis – narrowing
- Atresia – absence of
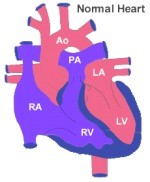
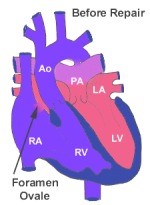
- Atrium and Ventricle - there are four chambers in the heart; both right and left having two each, one sitting above the other. The top chamber is called an atrium while the bottom chamber is called the ventricle.
- Mitral valve – this is the opening between the top and bottom chambers in the left side of the heart and acts as one-way valve.
- Tricuspid valve – this is the opening between the top and bottom chambers in the right side of the heart and acts as one-way valve.
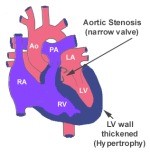
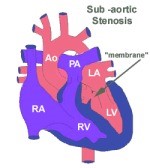
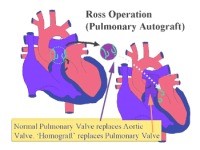
- Aortic valve – this is the opening that connects the left ventricle of the heart with the aorta, which is the major blood vessel that delivers oxygenated blood to the rest of the body. It acts as one-way valve.
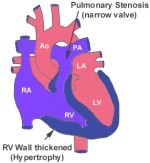
- Pulmonary valve – the valve in the opening that connects the right side of the heart to the vessels that delivers the used, oxygen depleted blood to the lungs. It acts as one-way valve.
- Septum – the wall that divides the right and left sides of the heart; the wall that divides both the atria is called the atrial septum and the wall that divides both the ventricles is called the ventricular septum.
There are many different types of CHD that fall into four common categories of congenital defects:
Obstruction to blood flow
This occurs when either abnormally formed heart valves or major blood vessels block the flow of blood into or out of the heart such as:
- Congenital aortic stenosis
- Mitral valve stenosis
- Pulmonary valve atresia/stenosis
- Absent pulmonary valve syndrome
- Coarctation of aorta
- Interrupted aortic arch
Left to right shunt
In a normal heart, the heart is made up of four chambers, two on either side, left and right. In simple terms, the left and right side of the heart are kept separated. The right side of the heart is responsible for receiving "used" blood (blood with reduced oxygen, which is blue) from the rest of the body and delivering it to the lungs. The left side of the heart is responsible for oxygen-rich blood (red blood) from the lungs and sending it out to the rest of the body.
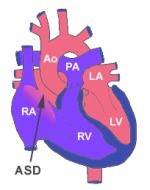
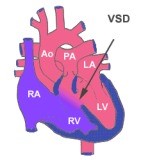
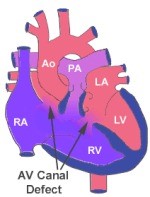
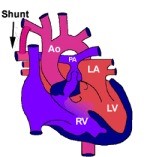
However, in left to right shunt types of CHD, the blood flows from left side of heart into right side of heart. This is due to abnormal connection between right and left side of the heart. This results in the right side becoming overloaded with an "extra volume" of blood. When this happens, it results in too much blood flowing into the lungs.
Conditions where this occurs are as follows:
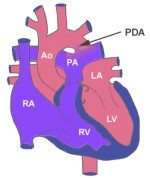
- Patent ductus arteriosus (PDA)
- Septal defects such as:
- Atrial septal defect (ASD)
- Ventricular septal defect (VSD)
- Atrio-Ventricular defect (AVSD)
- Aorto-pulmonary window
Right to left shunts
In right to left shunts, the blood now flows from the right side of the heart to the left. This is also due to abnormal connection between the right and left side of the heart. It results in a decreased flow of blood into the lungs, which means that the amount of “used”, or oxygen depleted blood pumped into the lungs to be re-oxygenated reduces. This condition is also called “cyanotic heart disease” as this condition causes a bluish colour of the skin (usually in the tip of fingers and toes) and mucous membranes (lips) due to low oxygen levels in the blood.
Conditions where this occurs are as follows:
- Teralogy of Fallot (TOF) which comprises four abnormalities:
- VSD
- Over-riding of the aorta
- Pulmonary stenosis
- Right ventricular hypertrophy
- Pulmonary atresia with intact VSD
- Pulmonary atresia with VSD
- Tricuspid atresia
- Ebstein's anomaly
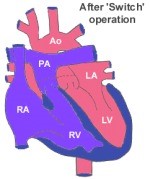
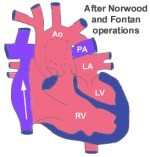
Complex cyanotic defects
These defects have more than one defect and are also known as “mixing defects”.
- Double outlet right ventricle
- Univentricular heart
- Total anomalous pulmonary venous connection
- Truncus arteriosus
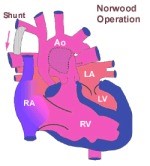
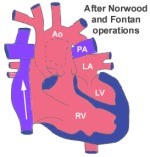
- Hypoplastic left heart syndrome
- Transposition of Great Arteries (TGA)
Medical and surgical treatments now offer these children an opportunity to grow and mature into adult life, an option that was not available in the past.