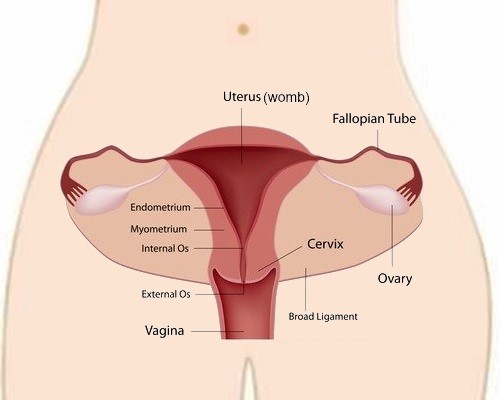
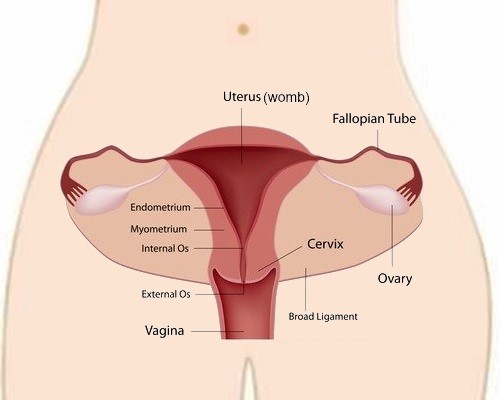
Cervical Cancer is cancer of the entrance to the uterus or womb. It starts when abnormal cells grow out of control in the transformation zone (the area where squamous cells and glandular cells meet).
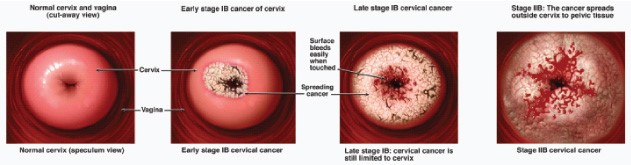
The cells do not suddenly transform into cancer; the normal cells in the cervix slowly change, which then turn it into cancer instead.
Long before there is a cancerous growth on the cervix, the cells of the cervix undergo changes that will eventually lead to cancer. These changes in the cells of the cervix are known as cervical dysplastic changes or cervical pre-cancer. Slowly and over time the abnormal and dysplastic cells increase in number and take over more and more normal tissue. Eventually when the dysplastic cells breach an important tissue layer, the basement membrane, the dysplastic growth has formally become a cancer.
During the pre-cancerous phase of dysplastic change, there are no noticeable symptoms, and the only reliable way to detect these pre-cancerous changes is to have a series of pap smear tests. This is the main reason to recommend having regular pap smear tests. The other reason regular pap smear tests work is that the pre-cancerous phase of change in the cervix extends over a significant period of time. In some studies, it has been estimated that it could take up to 10 years from the time the first pre-cancerous cell appears to the time that there is cancer on the cervix.
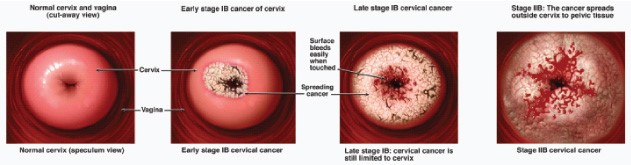
Cervical Cancer develops slowly. It develops from a few abnormal cells into a tumour over several years. That is why regular yearly pap smears are very effective in reducing a woman's risk of developing Cervical Cancer.
Cervical Cancer spreads outwards from the cervix to affect the bladder and rectum and it has a very prolonged and distinct pre-cancerous phase.
Papillomavirus is a key element in the development of Cervical Cancer. HPV is what is known as a DNA virus and although there are over 200 different subtypes, only a small handful are known as “high risk” HPV. They are known as “high risk” because if a woman is infected for a long time with a “high risk” HPV subtype it significantly increases the likelihood of her developing Cervical Cancer. There is a growing body of evidence that suggests that women who have never been exposed to HPV and who are vaccinated against it, have a much lower likelihood of ever developing Cervical Pre-Cancer or Cancer. HPV vaccines have been around for a sufficiently long time and with almost 200 million doses delivered worldwide, the World Health Organization has declared that the vaccine is safe and that all eligible women should consider vaccination. The HPV vaccination is also part of national vaccination programs for school children in countries such as Australia and Great Britain.
It is important at this point to emphasise that HPV infection is very common, almost like catching the common cold in humans, and that Cervical Cancer develops only in a very small percentage of the total number of HPV infections. The vast majority of women who are infected with HPV clear it effectively. The problem is that there is no effective way to know which women will effectively clear high-risk HPV and which will not, and among those that do not clear the viral infection, which women will go on to develop cervical cancer. This is why doctors recommend vaccination for everybody that is eligible.
With minimal effort, you can prevent Cervical Cancer effectively by getting your HPV vaccine and getting regular pap smear tests.