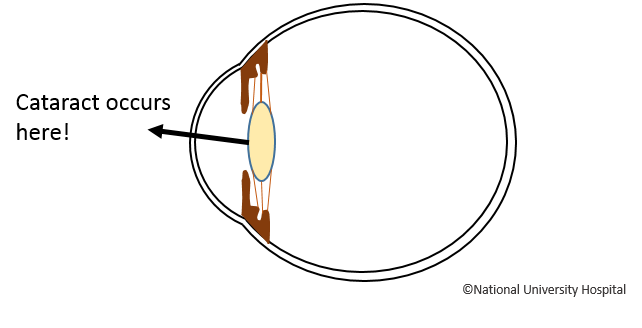
Early Cataracts are managed conservatively, and patients are usually prescribed glasses to aid their vision. When Cataracts affect one’s vision significantly, or in the case of those with other eye problems, Cataracts are managed by the surgical removal of the lens (Cataract extraction surgery).
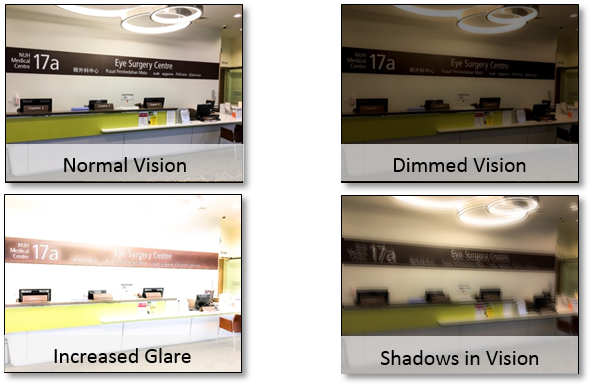
Cataract surgery is recommended when visual impairment affects daily living (dressing, navigating, cooking, showering, etc., or when patients have challenges with their vision as the Cataract becomes more severe. There is no absolute cut-off age for Cataract surgery.
If left untreated, Cataracts cause progressive loss of vision and eventually reversible blindness. In uncommon circumstances, it may lead to acute angle closure.
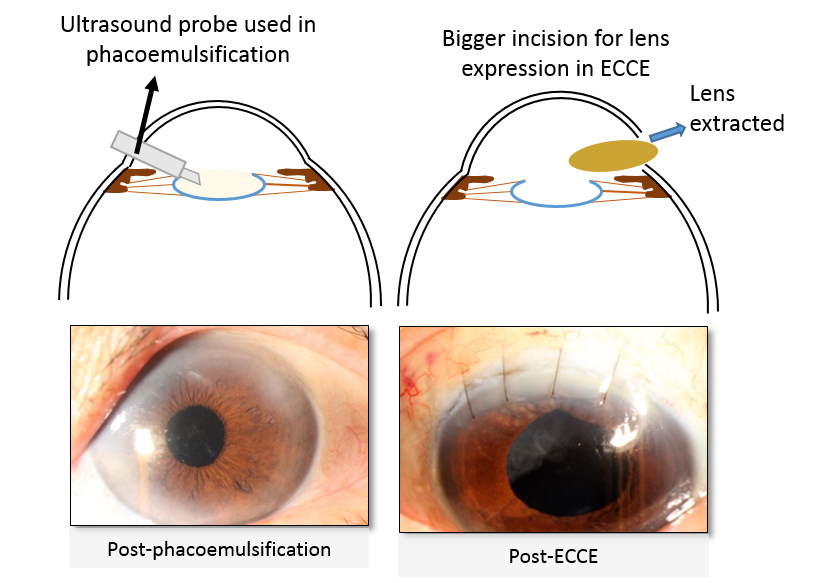
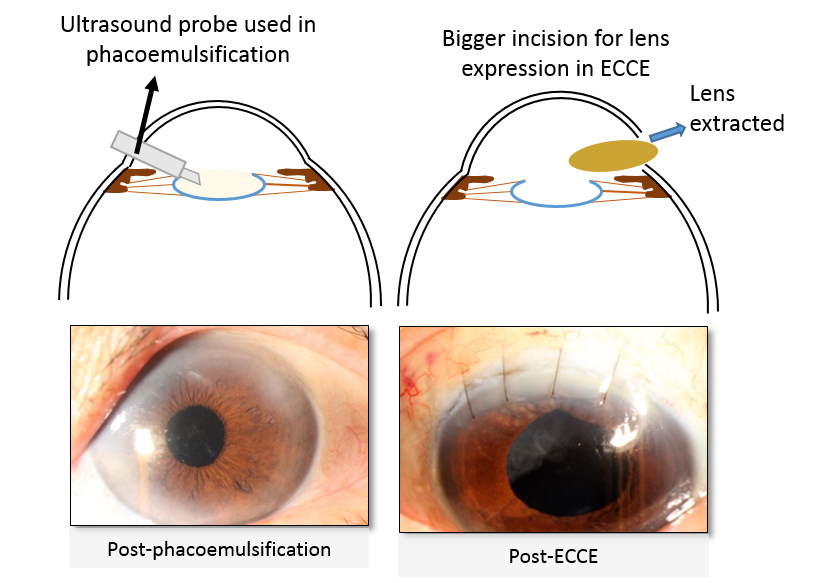
The most common form of Cataract surgery is phacoemulsification. The procedure takes about 20-minutes and can be performed under local anaesthesia as a day surgery.
Patients with more advanced Cataracts may undergo a more traditional surgery known as extracapsular Cataract extraction (ECCE). This surgery is about half an hour long and requires a larger incision. Visual rehabilitation will take longer and sutures may need to be removed about one to two months after surgery.
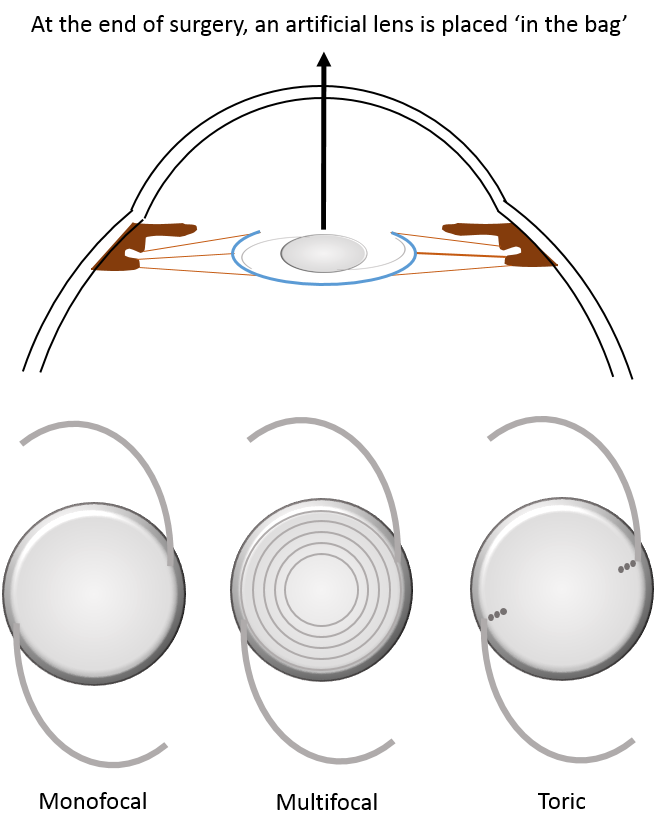
Cataract surgery involves removing your existing lens and replacing it with an intraocular lens with refractive power correction. Typically, a monofocal lens which corrects vision for distance only is used.
You must inform your surgeon if you have had laser refractive surgery performed (e.g. LASIK, PRK, epi-LASIK, SMILE) previously. Please bring along records of your previous treatment. This information is very important in ensuring accurate IOL calculation.
You will also need to stop wearing contact lens (at least one week for soft lens and at least two weeks for hard lens) prior to undergoing IOL calculation for surgical planning.
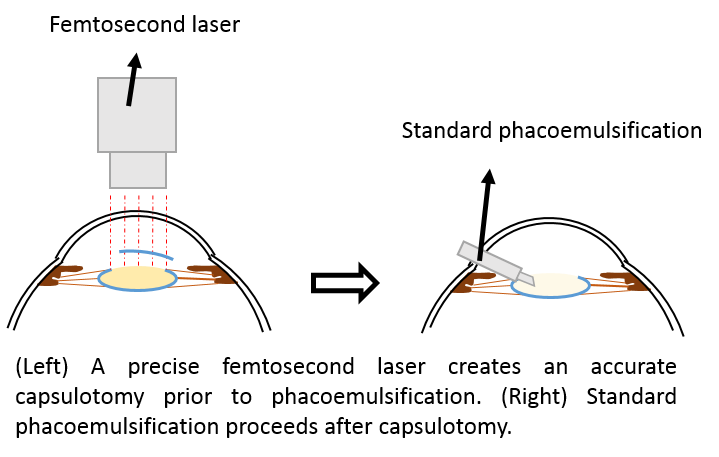
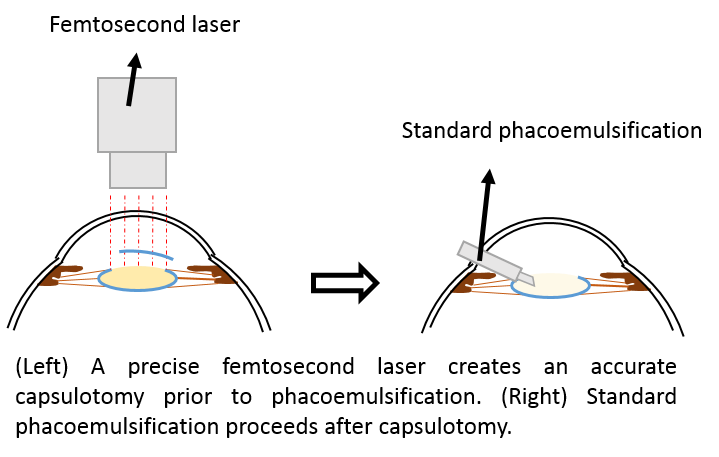
Femtosecond Laser-Assisted Cataract Surgery (FLACS)
FLACS is the latest form of Cataract extraction surgery where a precise laser replaces some, but not all, steps of standard phacoemulsification. The laser creates an opening in the anterior lens capsule, and softens the lens nucleus. It aims to reduce damage to the inner surface of the cornea and increase precision of intraocular lens placement.
The laser will first be performed at a separate machine, before the patient is transferred to the surgical bed for completion of the Cataract surgery. Your surgeon will need to evaluate your suitability for this procedure.
There are many factors affecting visual outcome after Cataract surgery. They include the amount of spectacle power correction after surgery, the amount of inflammation, and the wound healing process. It would be best to discuss this with your eye doctor.
The complications of FLACS is similar to that of standard phacoemulsification in major clinical trials. Risks include anterior capsule tear and tags, which increase the risk of posterior capsule rupture. After the surgery, there may be swelling of the back of the eye (macula edema), or raised intraoperative pressure.
FLACS may be beneficial for patients with less healthy corneas. It is not currently recommended as a standard procedure for all Cataract surgeries. The decision for FLACS should be discussed with your eye doctor.

As Cataract surgery is normally done as a day surgery procedure, patients are usually discharged on the same day, a few hours after surgery. They would be started on an eye drop and reviewed in the clinic one day, one week, and one month after the operation. Patients who undergo ECCE may require suture removal one to two months after the surgery.
After the operation, patients are given an eye shield to be used when sleeping. Patients are advised not to rub their eyes and to keep the affected eye clean and dry.