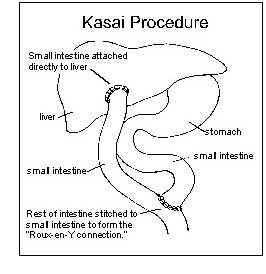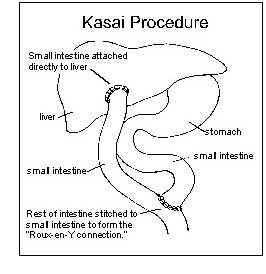
The treatment for Biliary Atresia is an operation called the Kasai Procedure. A paediatric surgeon will remove the blocked bile ducts outside the liver and connect a loop of small intestine directly to the liver. This allows bile to flow from the liver directly into the intestine. This segment of intestine that connects to the liver forms a Y connection and is called a Roux-en-Y hepatoportojejunostomy, also known as Kasai Procedure.
If the Kasai Procedure is successful in draining bile from the liver with complete disappearance of the jaundice, the child may live for many years and grow normally. When bile flow is only partly restored by surgery, the complications of cirrhosis will gradually develop and the child will eventually need a liver transplant. Some children may never need a liver transplant, but those who still experience no bile flow after undergoing the Kasai Procedure will require a liver transplant.
Adequate bile flow is needed for the digestion and absorption of dietary fats and fat-soluble vitamins such as vitamins A, B, E and K. When bile flow is reduced, the child might experience poor growth and have malnutrition. Special formulas containing medium-chain triglycerides (an easily-digested form of dietary fat), and water-soluble vitamin supplements are often prescribed to maximise the child's growth and development.
About 50% to 60% patients will achieve clearance of jaundice following the Kasai Procedure1. It is possible for these patients to survive more than 20 years on their native liver after undergoing the Kasai operation during early infancy. However, 60.5% of them may suffer from progressive liver-related complications2.
Long-term complications following Kasai Procedure are cholangitis and portal hypertension.
Cholangitis occurs when bacteria normally found in the small intestine migrate up the Roux-ex-Y, causing an infection. Signs of cholangitis include fever, increased jaundice and lighter colouration of stools. Antibiotics are needed to treat cholangitis or prevent it from happening.
Formation of scar tissue within the liver may cause hardening of the liver and a condition known as portal hypertension. Portal hypertension refers to the increased pressure in the veins connecting the intestines and spleen to the liver. Complications of portal hypertension include problems with bleeding and clotting, enlarged weak veins in the oesophagus and stomach and accumulation of fluid in the abdominal cavity called ascites.
When these complications can no longer be treated effectively with medication, the child is referred for liver transplantation. Liver transplantation is highly successful in the long-term treatment of children with Biliary Atresia with an overall survival of more than 90%3.
The child will be monitored and the follow-up continues until adulthood. Liver transplantation may be indicated for those cases who develop decompensated liver disease and its complications. Following liver transplantation, survival in these children is more than 89.3% at one year.