The treatments for Arrhythmias include either one or a combination of:
Lifestyle changes
- Refraining from smoking
- Avoiding activities that trigger the Arrhythmia
- Staying away from stimulants including caffeine, alcohol, certain cough or cold medications
Medication
- Anti-arrhythmic drugs that control the heart rate
- Anti-coagulant or anti-platelet therapy that reduces the risk of blood clot formation in your heart
Surgery
- Implantation of devices such as pacemakers, defibrillators, or Ventricular Assist Devices (VADs)
- Electrophysiology Study (EPS) with radiofrequency
Your cardiologist will recommend the type of treatment depending on the type, cause and condition of the disease.
Pacemakers, Defibrillators and Cardiac Implants
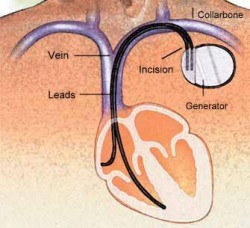
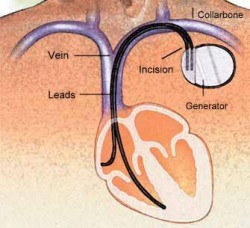
Pacemakers

Pacemakers are devices that help to stabilise the heart’s rhythm and are usually implanted into the heart when the heart rate is too slow.
The pacemaker device comprises of two parts:
- The pacemaker box (also known as the pulse generator) which contains the battery and electrical circuitry that controls the pacemaker.
- Wires (also called leads) that carry electrical impulses to the heart that allow it to beat at a rate determined by the pacemaker.
Pacemakers are:
- Reliable
- Unobtrusive
- Do not affect a patient’s daily activities
There are now "leadless" pacemakers without wires, that are used mainly in patients with no/limited vascular access.
Most patients notice an improvement in their conditions and symptoms after the insertion of a pacemaker.
Sometimes, pacemakers are implanted for patients with severe heart failure (see "Cardiac Resynchronisation Therapy") to improve their heart function.
Why do you need a cardiac pacemaker?
Excessively slow heart rhythms can severely affect the heart's ability to pump blood throughout the body.
This may cause symptoms such as:
- Fatigue
- Dizziness
- Shortness of breath
- Fainting
- In extreme circumstances, death
In such cases, your doctor may recommend a permanent pacemaker to be implanted.
What should you expect?
Though the procedure itself only takes about an hour, you will need to stay in hospital for one day for the pacemaker implantation.
Before the procedure:
- Some routine blood tests and electrocardiograms may be performed.
- You will be required to sign a consent form after your doctor explains the procedure and its risks.
- A small needle will be inserted in one of the veins on your hand to facilitate the injection of medication.
- You will be asked to fast on the night before the procedure.
During the procedure:
- The procedure is performed in the Invasive Cardiac Laboratory.
- Insertion is done under sedation and a local anaesthetic.
- A small incision is made in the skin just under the collarbone.
- A small “pocket” is created under the skin where the incision was made to house the pacemaker box.
- An insulated lead (wire) is then inserted through a vein in the upper chest.
- Guided by X-ray, it is threaded until its tip lies snugly within the heart.
- The other end of the lead is then connected to the pacemaker.
- Once the leads are positioned, an electrical test is done to ensure that the pacemaker is working correctly.
- The leads are then connected to the pacemaker and the incision is closed.
- At the end of the procedure, all that is visible is the closed incision line.
After the implantation:

On returning to the ward:
- You will be given regular antibiotic injections to reduce the risk of infection.
- Please inform the attending nurse if you experience pain at the implant site; painkillers can be prescribed.
On the following day:
- You will be sent for a chest X-ray to check the position of the pacemaker and wire, and to look for potential complications.
- The pacemaker will also be checked to programme by a technologist. This is done wirelessly.
- Most patients can be discharged one day after the procedure.
On returning home:
- You can resume most daily activities within a few days.
- Ensure that the wound on the chest remains dry.
- The waterproof dressing applied to the wound need not be changed till review in the clinic in 10 to 14 days.
- The stitches are absorbed naturally and do not need to be removed.
- Your doctor will arrange a schedule of periodic checks, and will electronically program the pacemaker's behaviour to suit your requirements.
What are the potential risks or complications?
The risks associated with the procedure are very low.
These include:
- Bleeding (from insertion of leads into the veins)
- Temporary injury to the lung
- Pneumothorax occurs infrequently when air leaks into the chest cavity causing the lung to collapse
- It is reversible and treated with the insertion of a tube into the chest to allow the lung to re-expand
- Infection of the pacemaker and lead systems
- This rarely occurs, and may require further antibiotics and removal of the pacemaker system
What should you do after the pacemaker implantation?
You should watch for fever, excessive pain, redness or swelling over the wound. Inform your doctor immediately if you have these symptoms.
Avoid excessive movement of the arm on the side of the pacemaker insertion. Avoid lifting the arm above your head and lifting more than 5 kg load for 2 weeks after the implantation.
Complete the course of antibiotic medication prescribed on discharge.
Remember to inform all your attending doctors that you have a permanent pacemaker. Some important reasons for this include:
- The use of short-wave diathermy, a form of treatment used to treat rheumatism, or diathermy used during surgery near where the pacemaker is should be avoided
- You should avoid have magnetic resonance imaging (MRI) tests done as well
If you have any queries regarding anything about the procedure or how to take care of yourself after the procedure, please contact your doctor.
Implantable cardiac defibrillators
These are used when patients are deemed to be at very high risk of sudden cardiac death from lethal heart rhythm disorders (Arrhythmias).
These sophisticated devices monitor the heart rhythm continuously and attempt to terminate these life-threatening rhythm disorders if they occur.
This can be through rapid pacing or delivery of an electrical shock to "reset" the heart to normal rhythm.
They are implanted the same way as pacemakers.
Implantable loop recorders
These are small devices inserted under the skin on the chest wall to monitor a patient's heart rhythm for prolonged periods of time (up to about 3 years).
They do not have any wires and may be used in certain situations such as recurrent fainting spells where a heart rhythm disorder is suspected as the cause but not documented previously.
Transcatheter left atrial appendage closure
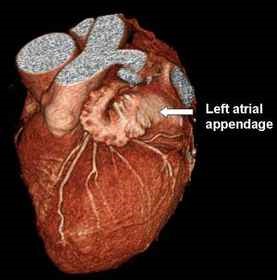
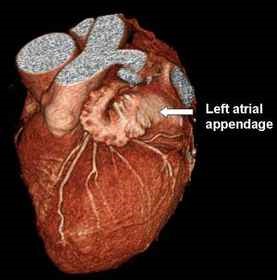
The left atrial appendage is an outpouching structure connected to the left atrium of the heart (left upper heart chamber). This is a normal heart structure and does not cause problems for most people. However, it can be a source of clot formation in patients with Atrial Fibrillation (AF).
The occurrence of AF in Singaporeans is approximately 1.5% but this is likely to increase as the population ages. It is the most common significant type of irregular heart rhythm in Singapore but most importantly, it is the biggest risk factor of strokes.
During AF, there is ineffective blood flow in the upper heart chambers leading to stagnation of blood in the left atrium. It has been shown that the majority of blood clots in patients with AF reside in this left atrial appendage.
Current evidence shows that the transcatheter left atrial appendage device closure is effective in reducing the risk of clot related complications associated with non-valvular causes of AF.
What are the options available to reduce the risks of stroke in patients with AF?
Though there are a variety of options available to reduce the risks of stroke in patients with AF, there is no single option that would be appropriate for every patient.
Your doctor will discuss these options with you and advise you on the option that is best suited for your condition. There are however several standard therapeutic options that you should be aware of. These include:
- Administration of blood thinners
- Open surgery to remove the left atrial appendage
- Transcatheter atrial appendage closure
What is transcatheter left atrial appendage device closure?
This is a procedure where device designed specifically to fit the left atrial appendage is delivered through a long, thin tube (catheter) to seal the orifice of the atrial appendage.
With time, tissue growth around and over the device will occur preventing further clot formation and migration.
How is this done?
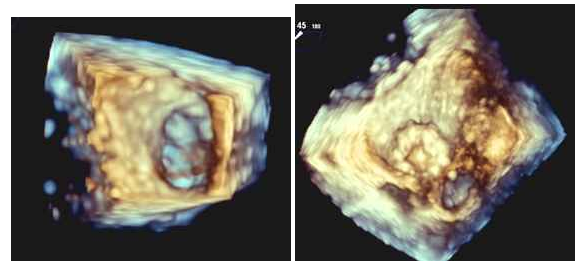
This procedure is done under general anaesthetic in a heart catheterisation laboratory.
It takes approximately 1-2 hours.
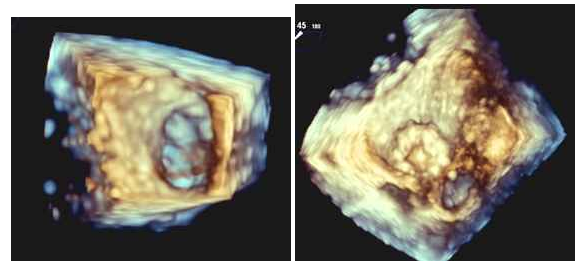
Transesophageal echocardiogram (a type of ultrasound for the heart) and fluoroscopy (a special X-ray using dye) are used to monitor the procedure.
A soft catheter (tube) is first introduced into the leg vein and then positioned across the atrial septum.
The left atrial appendage closure device is then delivered to its intended position and released.
What happens after the procedure?
- Once you are awake from the anaesthesia, you will be transferred to the cardiac monitoring unit for 24 hours.
- Most patients can be discharged 2-3 days after the procedure.
- The recovery time differs from patient to patient.
- You will be advised to avoid strenuous activities for 1 month after the procedure.
What are the risks involved in this procedure?
There are certain potential risks associated with any interventional procedure as well as risks specific to the device. Your doctor is the best person to provide you with accurate information and assessment of these risks. You should speak to him/her to address your concerns fully.
Potential risks include but are not limited to:
- Air embolus
- Allergic reactions to any medications given before, during or after the procedure
- Allergic reaction to the dye administered during the procedure
- Reaction to the drugs given for anaesthesia
- Arrhythmia during the procedure
- Bleeding
- Cardiac arrest – when the heart stops
- Cardiac tamponade - bleeding outside the heart between the heart muscle and the lining of the heart
- Death
- Device migration or embolisation
- Embolic events where particles of clot/air travel and obstruct blood flow
- Fever
- Foreign body embolisation
- High or low blood pressure
- Infections
- Heart attack
- Perforation
- Renal failure
- Stroke
- Blood clot formation
- Access site complications such as vessel injury
- Valve dysfunction