Background
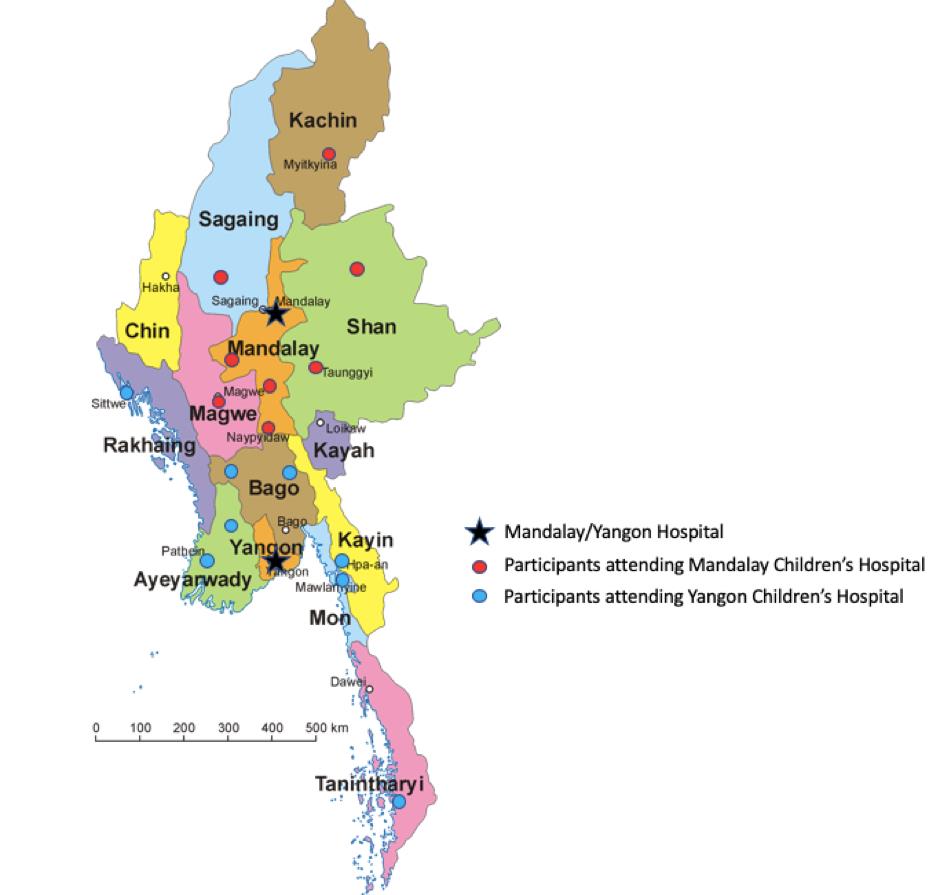
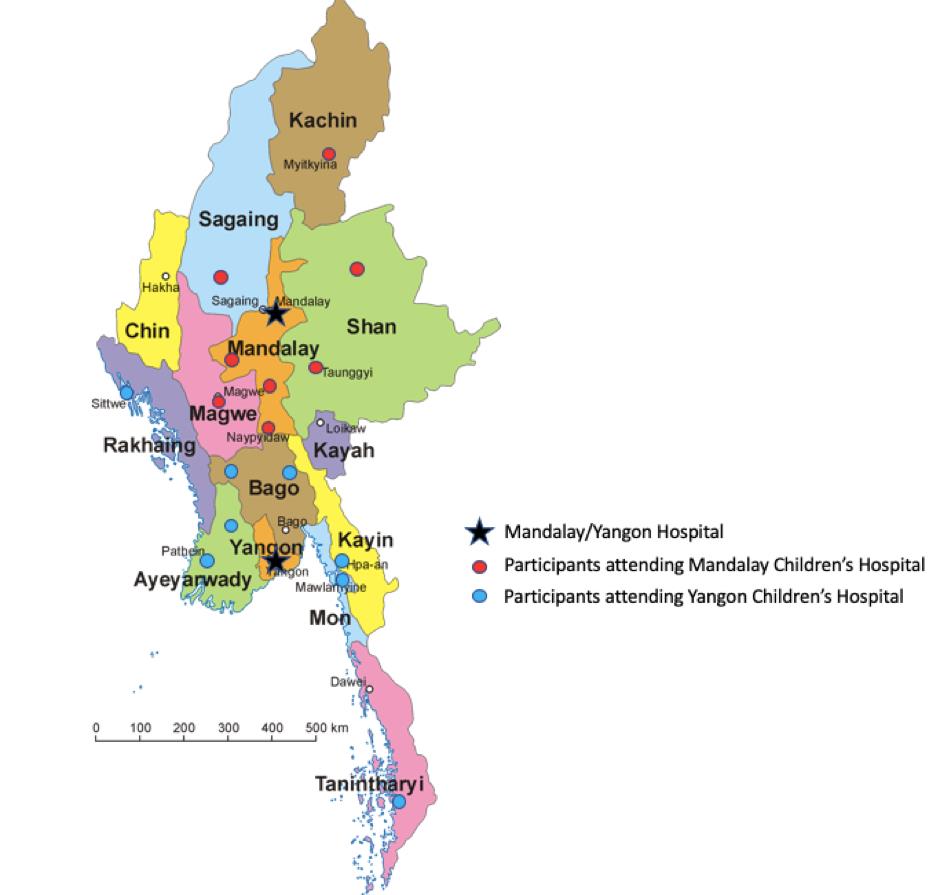
Myanmar is a large emerging country with a population of 55 million (2015 census), 18 million being under the age of 18 years old. It is divided into 15 states/division (provinces) and 345 towns are located within these 15 provinces.
There are two major centres that provide paediatric nephrology services in Myanmar; Yangon Children's Hospital and Mandalay Children's Hospital. Currently, most of the trained paediatric nephrologists are based in these two hospitals and these hospitals are the only two hospitals that provide chronic paediatric haemodialysis and peritoneal dialysis services. There are currently 12 paediatric nephrologists in Myanmar which provides paediatric nephrology coverage for the whole country.
Children in Myanmar develop acute kidney injury (AKI) secondary to sepsis, severe dehydration, glomerulonephritis, intravascular haemolysis, snake bites and nephrotoxin from Djenkol bean ingestion. These children have to be referred to one of the two main centres if they require dialysis. The children may be at locations hours away from the main city and transportation may not be reliable or could take a long duration of time. Some patients may also not be able to afford to travel to the main city for treatment, which would result in late presentation and increased mortality.
Currently, more than 10-12 children receive acute dialysis per month at Yangon Children's Hospital and Mandalay Children's Hospital. This is likely less than the actual number of patients needing acute dialysis as many may not be able to be transferred to the tertiary hospitals either due to transportation or financial constraints.
In each of the 15 states/divisions in Myanmar, there are 3-5 district hospitals (200 bedded) and 1-2 regional hospitals (providing secondary care) which are serviced by consultant paediatricians. We aim to train these consultant paediatricians and their paediatric nurses to perform acute peritoneal dialysis (PD) in order to initiate initial management prior to referral to the tertiary paediatric nephrology services or to perform PD in patients who are unable to be transferred.
Aim
The main aim of the course is to decrease the mortality rate from AKI in the paediatric population as well as to decrease the incidence of chronic kidney disease due to delayed management of patients with AKI.
Strategy
To equip paediatricians and paediatric nurses from regional and district hospitals with the ability to
recognise and manage acute kidney injury in paediatric patients including performing acute
peritoneal dialysis via training and education:
- To ensure understanding of the importance of AKI and its impact on health outcomes
- To improve knowledge of the aetiology and the diagnostic approach of AKI
- To be able to manage acute kidney injury in children
- To develop skills of acute peritoneal dialysis (PD) catheter insertion and to use acute PD in the management of acute kidney injury
- To understand the complications that can occur in acute PD and management strategies that can be used
Training course faculty and syllabus
The acute peritoneal dialysis training course in Myanmar was carried out in the two major cities in Myanmar - Yangon and Mandalay. The course was designed, organised and implemented by both the paediatric nephrology team from National University Hospital, Singapore together with the local International Pediatric Nephrology Association (IPNA)-trained paediatric nephrology team from Yangon Children's Hospital and Mandalay Children's Hospital. The local nephrology teams were important in ensuring the curriculum was made to include cases and topics that are relevant to the local community in Myanmar. The course was held in both English as well as Myanmar language to ensure complete understanding.
The Faculty from Singapore (left), the Yangon Faculty (middle) and the Mandalay Faculty (right)
Lecture topics were chosen to ensure participants had full understanding of:
- Acute kidney injury (AKI) definition, causes, diagnostic approach and management
- Long term implications of AKI and importance of AKI prevention
- Acute peritoneal dialysis (PD) - Principals of PD, technique of catheter insertion, prescription and managing complications
Each lecture was presented in English and translated to Burmese.
Practical sessions include workshops to allow participants opportunity to learn and perform acute peritoneal dialysis on mannequins, set up the PD circuit, PD prescriptions and monitoring. Eight additional workshops were run in small groups to cover all common cases of acute kidney injury in Myanmar (eg. AKI secondary to Djenkolism, snake bite, hypernatraemic dehydration) which allows participants to manage cases of AKI, practice performing peritoneal dialysis and manage complications of peritoneal dialysis. The workshops were conducted in both English and Burmese.

Participants
The participants were paediatricians and paediatric nurses from district and regional hospitals all over Myanmar. Participants from the south/lower Myanmar attended the course in Yangon and participants from upper Myanmar attended the course in Mandalay. Participants that attended came in pairs from the same hospital (paediatrician and nurse pair). There were 16 participants (eight paediatricians and eight nurses) that attended the course in Yangon and similarly 16 participants (eight paediatricians and eight nurses) that attended the course in Mandalay.
In addition to the official participants, the local paediatricians, post-graduate students and nurses were also welcome to attend the lectures and to observe the workshops.
In Yangon, all participants had no previous training in PD catheter insertion. From the pre-course assessment, the most common causes of AKI from the different states/divisions in Myanmar includes snake bites, dehydration due to gastroenteritis, nephrotoxins, acute glomerulonephritis and sepsis. All participants hope to gain further knowledge regarding AKI and managing AKI as well as using acute PD as a form of management of AKI.
In Mandalay, three participants had previous nephrology training and one participant had previous training in PD catheter insertion. Participants similarly hope to gain knowledge in PD catheter insertion, AKI diagnosis and management and to prevent chronic kidney disease in children. Main challenges that they face are financial constraints and available facilities.


Achievements
The training course has achieved its goal in educating the paediatricians and paediatric nurses from the district and regional hospitals on acute kidney injury and the use of acute peritoneal dialysis as a means of management. Participants were given supplies to perform acute PD at the end of the course.
The local nephrology team will also continue to support the district and regional paediatricians. The local nephrology team are willing to mentor them on an ongoing basis. Not only are the local nephrology team offering phone advice and referrals to the district and regional paediatricians, they are also willing to travel to the district/regional hospitals to assist in the paediatrician's first PD catheter.
This course was also a platform for the local Myanmar nephrologists to advocate for the use of acute peritoneal dialysis in children with AKI to the Myanmar Ministry of Health and Sports (MOHS). After the course, the MOHS has requested for a full report from the local nephrology team and they are agreeable to support further supplies of equipment (PD catheter and PD fluid) to sustain ongoing acute PD use in the regional and district hospitals.
During the course, it was also unravelled that some district hospitals lack certain facilities that is needed to improve health outcomes. For example, in the division of Magwe which has a high incidence of snake bite, the local general hospital does not have fresh frozen plasma (FFP) supplies. This is a needed therapy for coagulopathy seen in snake envenomation. After the course the local paediatricians are encouraged to speak to the medical superintendent to attempt to obtain necessary equipment to produce FFP.
Future Plans
The team plans to carry out another similar acute PD training course in the remote states in order to reach out to participants from further districts/regions.
Ongoing, we hope that the local nephrology team will be able to conduct similar regular acute PD training courses.
We will be collecting data from the district/regional paediatric team whenever a patient with AKI is commenced on acute PD. We hope to see that this course has brought about a management change to their practice and that it will decrease the mortality in the paediatric AKI patients as well as the chronic kidney disease rate.