POP occurs when the uterus or part of the vaginal canal becomes lax and protrudes out of its original position.
The prolapse is due to the progressive weakening of the supporting tissues of the uterus and the vagina in situations such as pregnancy and childbirth, especially difficult and prolonged labour.
The supporting tissues become even weaker when you enter the menopause and as you grow older. If you are involve in strenuous physical work, or suffer from chronic cough and constipation, you have an increased tendency to develop POP.
Other causes include congenital weakness of the pelvic floor muscles, ligaments and fascia, and collagen deficiency.
There are several degrees of severity of POP:
- Mild or 1st degree prolapse
When the prolapse is still within the vagina
- Moderate or 2nd degree prolapse
When the prolapse is just outside the vagina
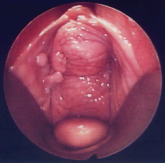
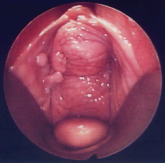
- Severe or 3rd and 4th degree prolapse
When the prolapse is completely outside the vagina
You may present with one or more types of prolapse:
When the top of the vagina supporting the bladder prolapses downwards into and outwards beyond the vagina.
When the bottom of the vagina supporting the rectum or small intestines respectively prolapses upwards into and outside of the vagina.
When the back of the vagina supporting the uterus prolapses into and beyond the vagina.
When there is prolapse of the uterus and vagina, including the bladder, completely outside the vagina.
When the back of the vagina prolapsea into and outside of the vagina after a previous hysterectomy.