Thyroid Eye Disease (TED) is an autoimmune disease associated with thyroid hormone dysfunction. It is mainly associated with an over-active thyroid due to Graves' disease, although it does sometimes occur in people with an under-active or normally functioning thyroid. The eyes are particularly vulnerable to Graves' eye disease, because the autoimmune attack often targets the eye muscles and connective tissue within the orbital socket. This likely occurs because the tissues within the orbit contain proteins that appear similar to the immune system as those of the thyroid gland. As a result of the autoimmune attack, the eye muscles and fatty tissue behind the eye become inflamed. This can cause the eyes to be pushed forward and the eyelids to be pulled upwards to some degree, giving rise to ‘staring’ or ‘bulging’ eyes. In the active state, the eyes feel painful and tight, and the eyes and eyelids often become swollen and red. In inactive or chronic phase, the extraocular muscles may become swollen and stiff, resulting in double vision. This condition is often seen among the middle-aged and elderly and is the most common cause of a prominent, wide-eyed staring appearance. If the condition is severe, it may lead to the inability to close the eyes when you sleep. Such severe protrusion of the eyeball that causes a ‘bug-eyed’ appearance is accompanied with a constant pressure and pain sensation, and may choke the optic nerve and even cause blindness. In addition to visual loss, the resultant disfiguration may psychologically and socially affect the patient. |
What are the signs & symptoms of Thyroid Eye Disease? Apart from activity, TED is also classified based on severity (mild, moderate or severe). In mild cases of TED, patients may only complain of sensitive and dry eyes, associated with increased tearing. Some mild cases may have associated lid signs, namely lid retraction and lid lag. In moderate TED, the patient usually has worsening of soft tissue signs, with greater lid retraction and exophthalmos. The patient may also experience diplopia (double vision) outside 30 degrees of primary gaze. In severe TED, the patient may experience severe exposure keratopathy not amenable to conservative management, compressive optic neuropathy, or diplopia in primary gaze, or within 30 degrees of primary gaze. |
What are the treatment options for Thyroid Eye Disease? In the early active phases of the disease which usually lasts 1-2 years, conservative management may alleviate most symptoms although appearance remains the same. When vision is threatened, steroid or immunosuppressant therapy may be considered. For residual deformities – various forms of eyelid, eye muscle and orbital surgery usually help restore a more normal appearance. The Orbital Surgeon, the Neuro-ophthalmologist and the Thyroid specialist will usually come together as a team to help evaluate the patient and optimise medical treatment before surgical rehabilitation restores patient to a comfortable pre-morbid normal self. For all patients with TED, the following measures may prevent disease progression: - Symptomatic treatment of dry eyes including topical lubricants, sunglasses in bright sunlight or temporary punctal plugs.
- Give up smoking, both active and passive, in order to reduce the severity, duration of activity, degree of scarring, and risk of optic nerve involvement.
- Co-manage all patients with an endocrinologist, and ensure their thyroid disease is well-controlled at each visit.
Classifying the patient into active or inactive disease is very important from a management point of view – - Active disease requires immunosuppression, of which intravenous methylprednisolone is the treatment of choice.
- Steroid sparing immunosuppressant therapy, given in collaboration with the Rheumatology team, is considered for their steroid sparing effects especially in cases of persistent inflammation.
- External beam radiotherapy, given by radiation oncologists, may also be considered in those patients who have contraindications or intolerance to various forms of corticosteroid/steroid sparing agents, but generally avoided both in the young and the elderly, as well as those with diabetes.
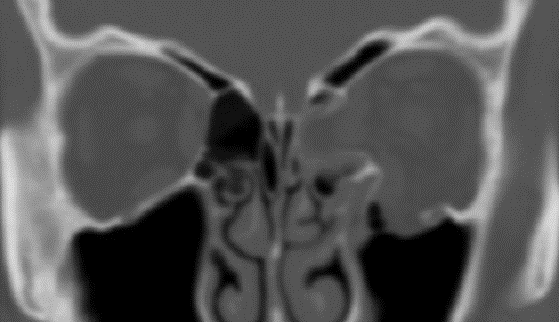
Surgical management for TED includes the following: - Orbital decompression and this may be done for several indications:
- Protrusion of the eyes
- Persistent congestion after immunosuppression
- Compressive optic neuropathy
- As a staging procedure, in preparation for strabismus or eyelid surgery
- Strabismus surgery - Surgery on the extraocular muscles is performed to correct the misalignment of the eyes.
- Eyelid surgery includes surgery to correct:
- Upper or lower lid retraction
- Upper or lower blepharoplasty (to remove excess skin and fat)
Thyroid eye disease remains a major clinical and therapeutic challenge. It has been shown to have a negative impact on psychosocial functioning and quality of life, even in mild cases. Fortunately, there are continued advances in the understanding of pathogenesis, risk-benefit profile of various medical and surgical interventions, making it a much more manageable disease compared to decades ago. The ultimate goal is early identification of TED, with effective halting and reversal of the active inflammatory process. The need for a patient-centered, multidisciplinary approach to these patients is important, to ensure careful and coordinated care for these patients. |