An Anal Fistula is a recurrent infection affecting the anus and occasionally the lower rectum. It causes considerable discomfort and disability to the sufferer of this chronic condition.
In Singapore, this condition is also known as the 'rat hole' (LaoShudong) amongst the Chinese community and traditional Chinese medical practitioners. It commonly affects economically active adults in the 3rd to 5th decades of life.
Although Anal Fistulas have been recognised for thousands of years, the treatment of the complex or recurrent Anal Fistula continues to challenge surgeons till today.
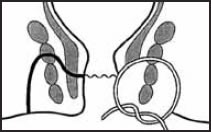
A fistula is a medical term describing an abnormal tract with two openings (internal and external) communicating between any two epithelium lined surfaces.
Therefore, an Anal Fistula is an abnormal tract communicating between the perianal area to the anal canal, and occasionally to the lower rectum.
Anal Fistula
Anal Fistulas and anal abscesses are separate phases along the spectrum of a common infective condition affecting the anus. The abscess represents the acute stage whereas the fistula is the representative of the chronic phase.
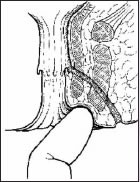
The anal canal is a muscular tube approximately 3 to 4 cm long, connecting the rectum to the anal verge. It is made up of 2 cylindrical muscle tubes called the outer and inner anal sphincter muscles. Anal glands are found in-between these two muscle tubes at the level of the dentate line (approximately 2 cm from the anal verge).

Anal Abscess Fig. 1

Anal Abscess Fig. 2
The role of these anal glands in humans is unknown.
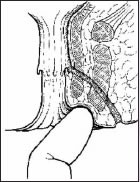
It is believed that the duct from the anal glands is blocked resulting in stasis, infection and subsequently abscess formation. Persistence of the infected anal gland and its duct results in the formation of an Anal Fistula.
As the duct from the infected anal gland leading into the anal canal is blocked, the accumulated pus may spread in other directions. It usually follows the path of least resistance. The path created will determine the type of Anal Fistula formed.
90% of all anal abscesses result from non-specific infection of the anal glands. We do not know why certain individuals are prone to this infection but approximately 25% to 30% of these patients with anal abscesses will eventually end up with an Anal Fistula.
Only people with susceptible anal glands can develop anal abscess and eventually Anal Fistula.
The formation of Anal Fistulas is totally unpredictable. The only way to prevent the disease is to reduce the incidence of an infection of the anal glands, which is the precursor to an Anal Fistula. Good perianal hygiene is an important step to prevent this uncomfortable condition.